Myasthenia gravis
Myasthenia gravis (MG) is a long-term neuromuscular junction disease that leads to varying degrees of skeletal muscle weakness.
[1] Most cases are due to immunoglobulin G1 (IgG1) and IgG3 antibodies that attack AChR in the postsynaptic membrane, causing complement-mediated damage and muscle weakness.
[21] The muscles that control breathing and limb movements can also be affected; rarely do these present as the first symptoms of MG, but develop over months to years.
Their medicine-induced MG symptoms were often severe with 29 patients developing respiratory failure that required mechanical ventilation.
[28] Non-statin cholesterol-lowering drugs, (e.g., nicotinic acid and the bile acid sequestrants drugs cholestyramine, colestipol, colesevelam, alirocumab, and evolocumab) have been used in patients without causing or worsening MG.[24] Ia antiarrhythmic agents: A type Ia antiarrhythmic agent (see Vaughan Williams classification), i.e., procainamide, which is used to treat cardiac arrhythmias, has caused respiratory failure in people with myasthenia gravis who, prior to being treated with it, did not have respiratory symptoms.
Local botulinum toxin A injections for cosmetic purposes have on occasion caused weaknesses in distant muscles, symptoms resembling ocular or generalized MG in individuals with subclinical MG, and exacerbations of previously controlled MG. Botulinum toxin A has also been used to treat spasmodic torticollis (i.e., involuntarily neck turning), blepharospasm (involuntary contraction of the eye lids), and other uncontrolled facial muscle spasms in people with myasthenia gravis without side effects or with only short-lived dysphagia or diplopia.
Botulinum toxin A treatment, it is suggested, is best avoided in people with myasthenia gravis but may be offered with caution to patients with mild or stable MG using gradual increases in its dosages and close monitoring.
There are two broad classes of these anesthetics: esters (i.e., procaine, cocaine, tetracaine benzocaine, and chloroprocaine) and amides (i.e. lidocaine, bupivacaine, etidocaine, levobupivacaine, mepivacaine, prilocaine, and ropivacaine).
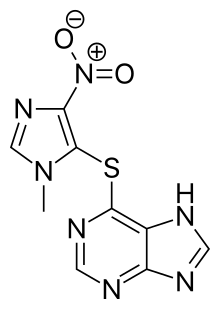
Based on these considerations, amide local anesthetics are strongly preferred over ester local anesthetics in patients with MG.[36][37] Other Drugs: Rare cases of MG exacerbations have been reported in patients treated with: 1) penicillins, i.e., ampicillin and amoxicillin; 2) anti-cancer medications, i.e., lorlatinib, nilotinib, imatinib (these three drugs are tyrosine kinase inhibitors that may also cause MG), dabrafenib, and trametinib; 3) antipsychotic drugs, i.e., chlorpromazine, pimozide, thioridazine, clozapine, olanzapine, haloperidol, quetiapine, risperidone, and olanzapine; 4) IFN-α (may also cause MG); and 5) the chemical element, lithium.
[45] Immunosuppressive therapy should be maintained throughout pregnancy, as this reduces the chance of neonatal muscle weakness, and controls the mother's myasthenia.
[46] About 10–20% of infants with mothers affected by the condition are born with transient neonatal myasthenia gravis (TNMG), which generally produces feeding and respiratory difficulties that develop about 12 hours to several days after birth.
[46][47] Myasthenia gravis can be difficult to diagnose, as the symptoms can be subtle and hard to distinguish from both normal variants and other neurological disorders.
[50] When diagnosed with MG, patient can be stratified into distinct subgroups based on the clinical features and serological status, e.g. affected muscle group, age of onset, thymic abnormalities, and profile of serum autoantibodies.
[20] If the diagnosis is suspected, serology can be performed: Muscle fibers of people with MG are easily fatigued, which the repetitive nerve stimulation test can help diagnose.
Jitter refers to the abnormal variation in the time interval between action potentials of adjacent muscle fibers in the same motor unit.
Blocking refers to the failure of nerve impulses to elicit action potentials in adjacent muscle fibers of the same motor unit.
[58] Applying ice for 2–5 minutes to the muscles reportedly has a sensitivity and specificity of 76.9% and 98.3%, respectively, for the identification of MG. Acetylcholinesterase is thought to be inhibited at the lower temperature, which is the basis for this diagnostic test.
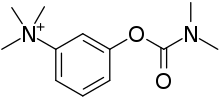
[59] This test requires the intravenous administration of edrophonium chloride or neostigmine, drugs that block the breakdown of acetylcholine by cholinesterase (acetylcholinesterase inhibitors).
[60] This test is no longer typically performed, as its use can lead to life-threatening bradycardia (slow heart rate) which requires immediate emergency attention.
[62] MRI of the cranium and orbits may also be performed to exclude compressive and inflammatory lesions of the cranial nerves and ocular muscles.
[71] Late-onset GSD-II (Pompe disease) and GSD-XV also have muscle weakness or fatigue with comorbidities of ptosis and ophthalmoplegia; as do many of the mitochondrial myopathies.
[79] Signs and symptoms of myasthenia presenting from infancy or childhood may be one of the congenital myasthenic syndromes, which can be inherited in either an autosomal dominant or recessive manner.
Medication consists mainly of acetylcholinesterase inhibitors to directly improve muscle function and immunosuppressant drugs to reduce the autoimmune process.
Both of these treatments have relatively short-lived benefits, typically measured in weeks, and often are associated with high costs, which make them prohibitive; they are generally reserved for when MG requires hospitalization.
[97][101] As thymomas are seen in 10% of all people with the MG, they are often given a chest X-ray and CT scan to evaluate their need for surgical removal of their thymus glands and any cancerous tissue that may be present.
[106] Monitoring of a person with MG is very important, as at least 20% of people diagnosed with it will experience a myasthenic crisis within two years of their diagnosis, requiring rapid medical intervention.
[1] In the early 1900s, 70% of detected cases died from lung problems; now, that number is estimated to be around 3–5%, an improvement attributed to increased awareness and medications to manage symptoms.
[19] In 1973, Patrick and Lindstrom used rabbits to show that immunization with purified muscle-like acetylcholine receptors caused the development of MG-like symptoms.
After the addition of pathogenic antibodies against the acetylcholine receptor and activation of the complement system, the neuromuscular co-culture shows symptoms such as weaker muscle contractions.
[111] Recent years, scientists have been working on finding the reliable biomarkers for MG to monitor the disease development and assess the severity.