Route of administration
An exception is topical administration, which generally means that both the application location and the effect thereof is local.
Furthermore, some application locations often classified as enteral, such as sublingual[6] (under the tongue) and sublabial or buccal (between the cheek and gums/gingiva), are taken up in the proximal part of the gastrointestinal tract without reaching the intestines.
In hospice care, a specialized rectal catheter, designed to provide comfortable and discreet administration of ongoing medications provides a practical way to deliver and retain liquid formulations in the distal rectum, giving health practitioners a way to leverage the established benefits of rectal administration.
[4][5] By this definition, topical administration also includes transdermal application, where the substance is administered onto the skin but is absorbed into the body to attain systemic distribution.
One such medication is the antibiotic vancomycin, which cannot be absorbed in the gastrointestinal tract and is used orally only as a treatment for Clostridioides difficile colitis.
This is the most reliable route, as in acutely ill patients the absorption of substances from the tissues and from the digestive tract can often be unpredictable due to altered blood flow or bowel motility.
[25] The oral route is limited to formulations containing small molecules only while biopharmaceuticals (usually proteins) would be digested in the stomach and thereby become ineffective.
In particular permeation enhancers,[27] ionic liquids,[28] lipid-based nanocarriers,[29] enzyme inhibitors and microneedles[30] have shown potential.
The bioavailability of oral administration is affected by the amount of drug that is absorbed across the intestinal epithelium and first-pass metabolism.
[33] The sublingual mucosa is highly permeable and thereby provides access to the underlying expansive network composed of capillaries, leading to rapid drug absorption.
[33] Intranasal absorption features low lipophilicity, enzymatic degradation within the nasal cavity, large molecular size, and rapid mucociliary clearance from the nasal passages, which explains the low risk of systemic exposure of the administered drug absorbed via intranasal.
[26] Upon contact with the skin, the drug penetrates into the dead stratum corneum and can afterwards reach the viable epidermis, the dermis, and the blood vessels.
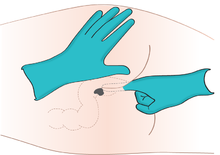
The term injection encompasses intravenous (IV), intramuscular (IM), subcutaneous (SC) and intradermal (ID) administration.
[38] Disadvantages of injections include potential pain or discomfort for the patient and the requirement of trained staff using aseptic techniques for administration.
[26] In general, only 20–50% of the pulmonary-delivered dose rendered in powdery particles will be deposited in the lung upon mouth inhalation.
[47] An inhaled powdery particle that is between 3 and 8 μm in diameter tend to largely deposit in the transitional zones of the lung by sedimentation.
[47] An inhaled powdery particle that is <3 μm in diameter is structurally predisposed to depositing primarily in the respiratory regions of the peripheral lung via diffusion.
[47] Particles that deposit in the upper and central airways are generally absorbed systemically to great extent because they are only partially removed by mucociliary clearance, which results in orally mediated absorption when the transported mucus is swallowed, and first pass metabolism or incomplete absorption through loss at the fecal route can sometimes reduce the bioavailability.
Neural drug delivery is the next step beyond the basic addition of growth factors to nerve guidance conduits.











- trachea (conducting zone)
- main bronchus (conducting zone)
- lobar bronchus (conducting zone)
- segmental bronchus (conducting zone)
- subsegmental bronchus (conducting zone)
- conducting bronchiole (conducting zone)
- terminal bronchiole (conducting zone)
- respiratory bronchiole (transitional respiratory zone)
- alveolar duct (transitional respiratory zone)
- alveolar sac (transitional respiratory zone)
- alveolus (transitional respiratory zone)


