Parathyroid hormone
Parathyroid hormone 1 receptors, activated by the 34 N-terminal amino acids of PTH, are present at high levels on the cells of bone and kidney.
Parathyroid hormone 2 receptors are present at high levels on the cells of central nervous system, pancreas, testes, and placenta.
[8] Disorders that yield too little or too much PTH, such as hypoparathyroidism, hyperparathyroidism, and paraneoplastic syndromes can cause bone disease, hypocalcemia, and hypercalcemia.
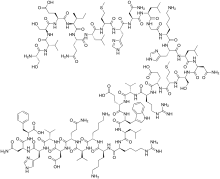
[9] The N-terminal fragment 1-34 of parathyroid hormone (PTH) has been crystallized and the structure has been refined to 0.9 Å resolution.
Binding stimulates osteoblasts to increase their expression of RANKL and inhibits their secretion of osteoprotegerin (OPG).
In the bone marrow, estrogen downregulates the proliferation of hematopoietic stem cells through an IL-7 dependent mechanism.
[11] Circulating parathyroid hormone only influences the reabsorption that occurs in the distal tubules and the renal collecting ducts[11] (but see Footnote[nb 1]).
[§ 1] Secretion of parathyroid hormone is determined chiefly by serum ionized calcium concentration through negative feedback.
In the parathyroid gland, high concentrations of extracellular calcium result in activation of the Gq G-protein coupled cascade through the action of phospholipase C. This hydrolyzes phosphatidylinositol 4,5-bisphosphate (PIP2) to liberate intracellular messengers IP3 and diacylglycerol (DAG).
A mild decrease in serum magnesium levels stimulates the reabsorptive activity PTH has on the kidneys.
[24] Hyperparathyroidism, the presence of excessive amounts of parathyroid hormone in the blood, occurs in two very distinct sets of circumstances.
A low level of PTH in the blood is known as hypoparathyroidism and is most commonly due to damage to or removal of parathyroid glands during thyroid surgery.
There are a number of rare but well-described genetic conditions affecting parathyroid hormone metabolism, including pseudohypoparathyroidism, familial hypocalciuric hypercalcemia, and autosomal dominant hypercalciuric hypocalcemia.
In osteoporotic women, administration of an exogenous parathyroid hormone analogue (teriparatide, by daily injection) superimposed on estrogen therapy produced increases in bone mass and reduced vertebral and nonvertebral fractures by 45–65%.
[35][36][37][38] Recombinant human parathyroid hormone is used in the treatment of osteoporosis in postmenopausal women at high risk of osteoporotic fractures.



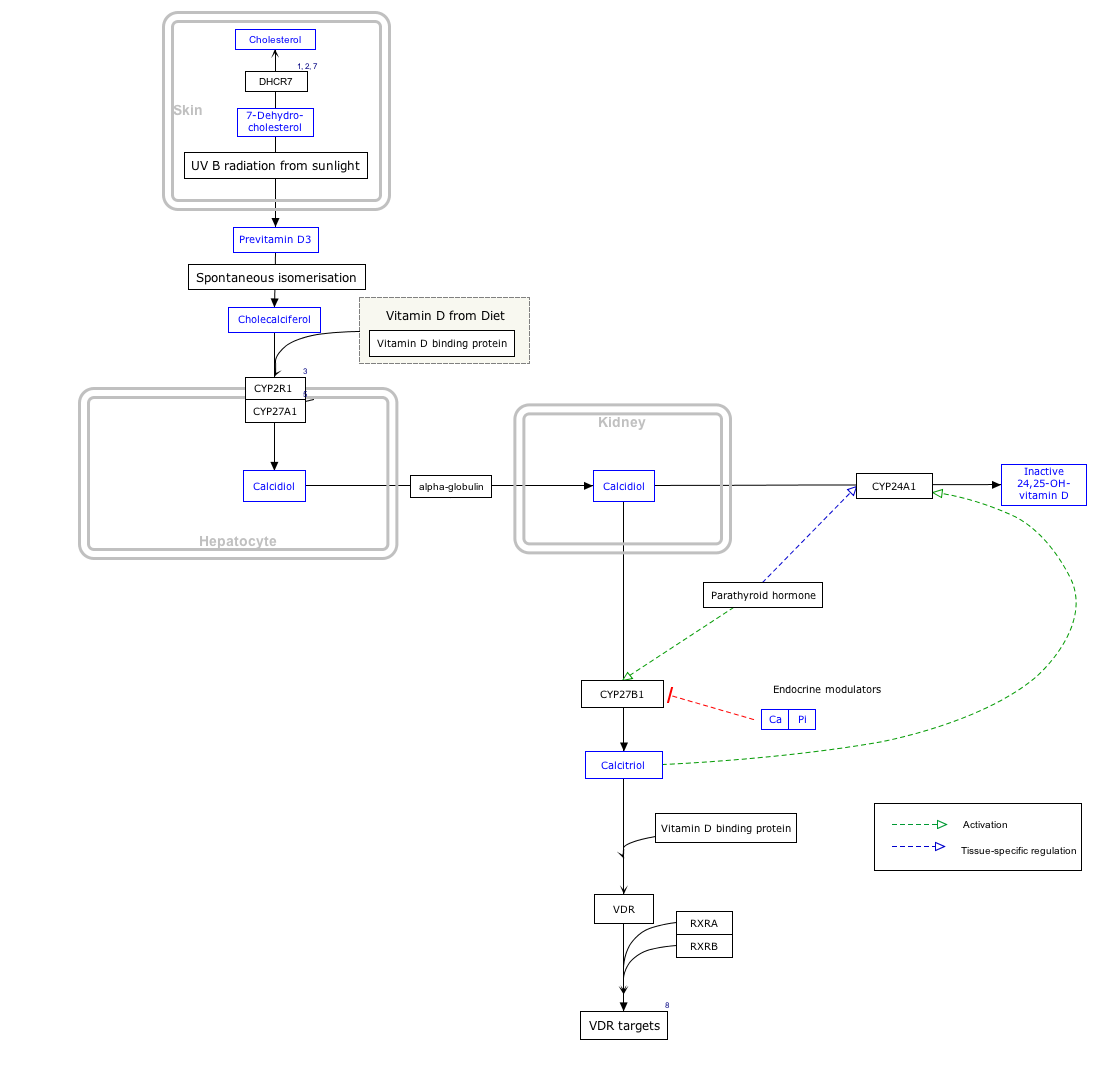
The widths of the red arrows indicating movement into and out of the plasma are roughly in proportion to the daily amounts of calcium moved in the indicated directions.
The size of the central square in not in proportion to the size of the diagrammatic bone, which represents the calcium present in the skeleton, and contains about 25,000 mmol (or 1 kg) of calcium compared to the 9 mmol (360 mg) dissolved in the blood plasma.
The differently colored narrow arrows indicate where the specified hormones act, and their effects (“+” means stimulates; “-“ means inhibits) when their plasma levels are high.
PTH is parathyroid hormone, 1,25 OH VIT D 3 is calcitriol or 1,25 dihydroxyvitamin D 3 , and calcitonin is a hormone secreted by the thyroid gland when the plasma ionized calcium level is high or rising.
The diagram does not show the extremely small amounts of calcium that move into and out of the cells of the body, nor does it indicate the calcium that is bound to the extracellular proteins (in particular the plasma proteins) or to plasma phosphate. [ 11 ] [ 12 ] [ 13 ] [ 14 ] [ 15 ]