Penicillin
[6] Fleming's student Cecil George Paine was the first to successfully use penicillin to treat eye infection (neonatal conjunctivitis) in 1930.
The purified compound (penicillin F) was isolated in 1940 by a research team led by Howard Florey and Ernst Boris Chain at the University of Oxford.
[9] Fleming explained in his 1929 paper in the British Journal of Experimental Pathology that "to avoid the repetition of the rather cumbersome phrase 'Mould broth filtrate', the name 'penicillin' will be used.
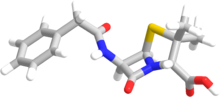
This side chain is connected to the 6-aminopenicillanic acid residue and results in variations in the antimicrobial spectrum, stability, and susceptibility to beta-lactamases of each type.
Penicillin V (phenoxymethylpenicillin) is produced by adding the precursor phenoxyacetic acid to the medium in which a genetically modified strain[dubious – discuss] of the penicillium fungus is being cultured.
This group of antibiotics is called "broad-spectrum" because they are active against a wide range of Gram-negative bacteria such as Escherichia coli and Salmonella typhi, for which penicillin is not suitable.
Penicillin G is licensed for use to treat septicaemia, empyema, pneumonia, pericarditis, endocarditis and meningitis caused by susceptible strains of staphylococci and streptococci.
[48] But penicillin can still enter Gram-negative species by diffusing through aqueous channels called porins (outer membrane proteins), which are dispersed among the fatty molecules and can transport nutrients and antibiotics into the bacteria.
Alternatively, flucloxacillin is a modified penicillin that has activity against β-lactamase-producing bacteria due to an acyl side chain that protects the beta-lactam ring from β-lactamase.
In 1940, they discovered that unsusceptible bacteria like Escherichia coli produced specific enzymes that can break down penicillin molecules, thus making them resistant to the antibiotic.
For example, resistance to vancomycin in S. aureus is due to additional peptidoglycan synthesis that makes the cell wall much thicker preventing effective penicillin entry.
A common case is found in Streptococcus pneumoniae where there is mutation in the gene for PBP, and the mutant PBPs have decreased binding affinity for penicillins.
[44] In MRSA, mutations in the genes (mec system) for PBP produce a variant protein called PBP2a (also termed PBP2'),[69] while making four normal PBPs.
PBP2a has poor binding affinity for penicillin and also lacks glycosyltransferase activity required for complete peptidoglycan synthesis (which is carried out by the four normal PBPs).
[75] Starting in the late 19th century there had been reports of the antibacterial properties of Penicillium mould, but scientists were unable to discern what process was causing the effect.
[76] Scottish physician Alexander Fleming at St. Mary's Hospital in London (now part of Imperial College) was the first to show that Penicillium rubens had antibacterial properties.
[81] The importance of his work has been recognized by the placement of an International Historic Chemical Landmark at the Alexander Fleming Laboratory Museum in London on 19 November 1999.
[83] In 1930, Cecil George Paine, a pathologist at the Royal Infirmary in Sheffield, successfully treated ophthalmia neonatorum, a gonococcal infection in infants, with penicillin (fungal extract) on November 25, 1930.
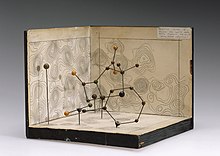
[84][85][86] In 1940, Australian scientist Howard Florey (later Baron Florey) and a team of researchers (Ernst Chain, Edward Abraham, Arthur Duncan Gardner, Norman Heatley, Margaret Jennings, Jean Orr-Ewing and Arthur Gordon Sanders) at the Sir William Dunn School of Pathology, University of Oxford made progress in making concentrated penicillin from fungal culture broth that showed both in vitro and in vivo bactericidal action.
[90] The first successful use of pure penicillin was in 1942 when Fleming cured Harry Lambert of an infection of the nervous system (streptococcal meningitis) which would otherwise have been fatal.
[100] In July 1943, the War Production Board drew up a plan for the mass distribution of penicillin stocks to Allied troops fighting in Europe.
[101] The results of fermentation research on corn steep liquor at the NRRL allowed the United States to produce 2.3 million doses in time for the invasion of Normandy in the spring of 1944.
After a worldwide search in 1943, a mouldy cantaloupe in a Peoria, Illinois market was found to contain the best strain of mould for production using the corn steep liquor process.
[96] Pfizer scientist Jasper H. Kane suggested using a deep-tank fermentation method for producing large quantities of pharmaceutical-grade penicillin.
[101] G. Raymond Rettew made a significant contribution to the American war effort by his techniques to produce commercial quantities of penicillin, wherein he combined his knowledge of mushroom spawn with the function of the Sharples Cream Separator.
During World War II, penicillin made a major difference in the number of deaths and amputations caused by infected wounds among Allied forces, saving an estimated 12–15% of lives.
[106] Availability was severely limited, however, by the difficulty of manufacturing large quantities of penicillin and by the rapid renal clearance of the drug, necessitating frequent dosing.
The chemical structure of penicillin was first proposed by Edward Abraham in 1942[87] and was later confirmed in 1945 using X-ray crystallography by Dorothy Crowfoot Hodgkin, who was also working at Oxford.
These were significant for their activity against β-lactamase-producing bacterial species, but were ineffective against the methicillin-resistant Staphylococcus aureus (MRSA) strains that subsequently emerged.
While the usage of glucose as a carbon source represses penicillin biosynthesis enzymes, lactose does not exert any effect and alkaline pH levels override this regulation.