Pyelonephritis
[3][5] Among people over the age of 65 the risk of death is about 40%, though this depends on the health of the elderly person, the precise organism involved, and how quickly they can get care through a provider or in hospital.
[9] Chronic pyelonephritis causes persistent flank or abdominal pain, signs of infection (fever, unintentional weight loss, malaise, decreased appetite), lower urinary tract symptoms and blood in the urine.
Hospital-acquired infections may be due to coliform bacteria and enterococci, as well as other organisms uncommon in the community (e.g., Pseudomonas aeruginosa and various species of Klebsiella).
[9] E. coli can invade the superficial umbrella cells of the bladder to form intracellular bacterial communities (IBCs), which can mature into biofilms.
These biofilm-producing E. coli are resistant to antibiotic therapy and immune system responses, and present a possible explanation for recurrent urinary tract infections, including pyelonephritis.
Specifically, the presence of nitrite and white blood cells on a urine test strip in patients with typical symptoms are sufficient for the diagnosis of pyelonephritis, and are an indication for empirical treatment.
[9] Where available, a noncontrast helical CT scan with 5 millimeter sections is the diagnostic modality of choice in the radiographic evaluation of suspected nephrolithiasis.
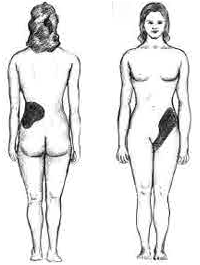
[19] In patients with recurrent ascending urinary tract infections, it may be necessary to exclude an anatomical abnormality, such as vesicoureteral reflux or polycystic kidney disease.
[22] Acute pyelonephritis is an exudative purulent localized inflammation of the renal pelvis (collecting system) and kidney.
The kidney parenchyma presents in the interstitium abscesses (suppurative necrosis), consisting in purulent exudate (pus): neutrophils, fibrin, cell debris and central germ colonies (hematoxylinophils).
[citation needed] Chronic pyelonephritis implies recurrent kidney infections and can result in scarring of the renal parenchyma and impaired function, especially in the setting of obstruction.
[10] In people who experience recurrent urinary tract infections, additional investigations may identify an underlying abnormality.
[26] In children at risk for recurrent urinary tract infections, not enough studies have been performed to conclude prescription of long-term antibiotics has a net positive benefit.
[28] In people suspected of having pyelonephritis, a urine culture and antibiotic sensitivity test is performed, so therapy can eventually be tailored on the basis of the infecting organism.
[15] A 2018 systematic review recommended the use of norfloxacin as it has the lowest rate of side effects with a comparable efficacy to commonly used antibiotics.
[29] In people who do not require hospitalization and live in an area where there is a low prevalence of antibiotic-resistant bacteria, a fluoroquinolone by mouth such as ciprofloxacin or levofloxacin is an appropriate initial choice for therapy.
The treatment regimen is selected based on local resistance data and the susceptibility profile of the specific infecting organism(s).
[30] Intravenous fluids may be administered to compensate for the reduced oral intake, insensible losses (due to the raised temperature) and vasodilation and to optimize urine output.
Removal of the kidney is the best surgical treatment in the overwhelming majority of cases, although polar resection (partial nephrectomy) has been effective for some people with localized disease.
[citation needed] The word pyelonephritis is formed by the Greek roots pyelo- from πύελος (púelos) renal pelvis and nephro- from νεφρός (nephrós) kidney together with the suffix -itis from -ῖτις (-itis) used in medicine to indicate diseases or inflammations.