Rasmussen syndrome
In the long term, most patients are left with some epilepsy, paralysis and cognitive problems, but the severity varies considerably.
[4] However, more recent studies report the presence of autoantibodies against the NMDA-type glutamate receptor subunit GluRepsilon2 (anti-NR2A antibodies) in a subset of patients with Rasmussen's encephalitis.
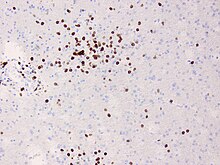
[6] By sequencing T cell receptors from various compartments it could be shown that RE patients present with peripheral CD8+ T-cell expansion which in some cases have been proven for years after disease onset.
[9][12] During the residual stage of the illness when there is no longer active inflammation, treatment is aimed at improving the remaining symptoms.
Standard anti-epileptic drugs are usually ineffective in controlling seizures, and it may be necessary to surgically remove or disconnect the affected cerebral hemisphere, in an operation called hemispherectomy or via a corpus callosotomy.
This usually results in further weakness, hemianopsia and cognitive problems, but the other side of the brain may be able to take over some of the function, particularly in young children.
[1][9] It is named for the neurosurgeon Theodore Rasmussen (1910–2002), who succeeded Wilder Penfield as head of the Montreal Neurological Institute, and served as Neurosurgeon-in-Chief at the Royal Victoria Hospital.