Theories of general anaesthetic action
General anaesthetics have been widely used in surgery since 1842 when Crawford Long for the first time administered diethyl ether to a patient and performed a painless operation.
[4] However, for certain intravenous anaesthetics, such as propofol and etomidate, the main molecular target is believed to be GABAA receptor, with particular β subunits playing a crucial role.
[1][5][6][7] A nonspecific mechanism of general anaesthetic action was first proposed by Emil Harless and Ernst von Bibra in 1847.
In 1899 Hans Horst Meyer published the first experimental evidence of the fact that anaesthetic potency is related to lipid solubility.
[12] Meyer compared the potency of many agents, defined as the reciprocal of the molar concentration required to induce anaesthesia in tadpoles, with their olive oil/water partition coefficient.
He found a nearly linear relationship between potency and the partition coefficient for many types of anaesthetic molecules such as alcohols, aldehydes, ketones, ethers, and esters.
From the correlation between lipid solubility and anaesthetic potency, both Meyer and Overton had surmised a unitary mechanism of general anaesthesia.
Based on this theory, in 1954 Mullins suggested that the Meyer-Overton correlation with potency can be improved if molecular volumes of anaesthetic molecules are taken into account.
For proteins, one reason that more polar general anaesthetics could be less potent is that they have to cross the blood–brain barrier to exert their effect on neurons in the brain.
This mechanism is also nonspecific because the potency of the anaesthetic is determined not by its actual chemical structure, but by the positional and orientational distribution of its segments and bonds within the bilayer.
A slightly different detailed molecular mechanism of how bilayer perturbation can influence the ion channel was proposed in the same year.
Recently super resolution imaging showed direct experimental evidence that volatile anesthetics disrupt the ordered lipid domains as predicted.
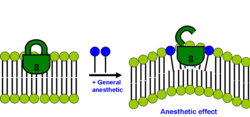
[38] These observations were important because they demonstrated that general anaesthetics exert their effect non-specifically including when binding to proteins.
A number of experimental and computational studies have shown that general anaesthetics could alter the dynamics in the flexible loops that connect α-helices in a bundle and are exposed to the membrane-water interface of Cys-loop receptors.
[43][44][45][46][47][48] The main binding pockets of general anaesthetics, however, are located within transmembrane four-α-helix bundles of Cys-loop receptors.
[53] Strong activation of tonic GABAA receptor conductance by clinical concentrations of propofol has been confirmed with electrophysiological recordings from hippocampal CA1 neurons in adult rat brain slices.
[55] Electrophysiological experiments with amnestic concentrations of etomidate have also shown enhancement of tonic GABAA conductance of CA1 pyramidal neurons in hippocampal slices.
[56] Potent activation of GABAA receptor-mediated inhibition with resulting strong depression of firing rates of neocortical neurons has also been demonstrated for clinical concentrations of volatile anesthetics such as isoflurane, enflurane and halothane.
[57] The enhancement of GABAA receptor activity is unlikely to be the only mechanism to account for the wide range of behavioural effects of general anaesthetics.
Alternatively, inhibition of glutamate-gated N-methyl-D-aspartate receptors by ketamine, xenon, and nitrous oxide provides a mechanism of action in keeping with a predominant analgesic profile.
[1] This means that optical isomers partition identically into lipid, but have differential effects on ion channels and synaptic transmission.
All general anaesthetics induce immobilization (absence of movement in response to noxious stimuli) through depression of spinal cord functions, whereas their amnesic actions are exerted within the brain.
According to the Meyer-Overton correlation the anaesthetic potency of the drug is directly proportional to its lipid solubility, however, there are many compounds that do not satisfy this rule.
[69] Good example of non-immobilizers are halogenated alkanes that are very hydrophobic, but fail to suppress movement in response to noxious stimulation at appropriate concentrations.
Experimental studies have shown that general anaesthetics including ethanol are potent fluidizers of natural and artificial membranes.
A plot of chain length vs. the logarithm of the lipid bilayer/buffer partition coefficient K is linear, with the addition of each methylene group causing a change in the Gibbs free energy of -3.63 kJ/mol.
[31][74] In short-chain alkanols (A) segments of the chain are rather rigid (in terms of conformational enthropy) and very close to hydroxyl group tethered to aqueous interfacial region ("buoy").
Efficiency of pressure redistribution decreases as the length of hydrocarbon chain increases until anaesthetic potency is lost at some point.
It was proposed that polyalkanols (C) will have anaesthetic effect similar to short-chain 1-alkanols if the chain length between two neighbouring hydroxyl groups is smaller than the cutoff.
[75] This idea was supported by the experimental evidence because polyhydroxyalkanes 1,6,11,16-hexadecanetetraol and 2,7,12,17-octadecanetetraol exhibited significant anaesthetic potency as was originally proposed.