Thymidine kinase in clinical chemistry
In clinical chemistry it has been suggested as a proliferation marker for prognosis, verification of diagnosis, control of treatment (particularly as a companion diagnostic) and follow-up of malignant disease.
It is present during cell division in much higher concentrations than TK2 and it is released in quantities that completely dominate the thymidine kinase activity in blood and other body fluids.
This second route is used by the cell under normal conditions, and it is sufficient to supply thymidine monophosphate for DNA repair.
[29] The main fraction of the active enzyme in the circulation has a molecular weight of 730 kD and is probably bound in a complex to other proteins.
[30] Thymidine kinase 1 (TK1) levels in serum or plasma may be measured based on their enzymatic activity or in terms of mass using immunoassays.
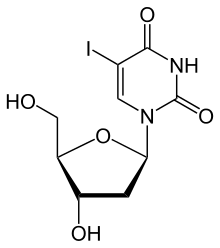
The oldest commercially available technique uses iodo-deoxyuridine (idoxuridine) wherein a methyl group in thymidine has been replaced with radioactive iodine.
After decantation and washing the radioactivity of the aluminum oxide gives a measure of the amount of thymidine kinase in the sample.
It is considerably more sensitive than the previous enzymatic methods and may be, therefore, more suitable for use with solid tumors where lower elevations of TK1 are found in body fluids.
This technique utilizes natural thymidine as substrate and can also determine deoxycytidine kinase simultaneously with TK1.
[40][41][42] Immunoassays have advantages over enzyme activity methods in that they can measure TK1 isoforms that are enzymatically inactive plus that they are unaffected by serum TK1 inhibitors.
The treated samples are added to a microtiter plate coated with anti TK 210 monoclonal antibodies.
After further washing, the color is developed with streptavidin labelled horse radish peroxidase with TMP as substrate.
A microchip electrophoresis immunoaffinity assay for determination of serum thymidine kinase concentration has been described.
[38][68][69] A very interesting case is the myelodysplastic syndrome: some rapidly change to acute leukemia, whereas others remain indolent for very long time.
The increases in serum TK1 activity levels in subjects with solid tumors are not as large as they are for hematologic malignancies.
The experimental method first developed by Gronowitz et al.[31] used quantities of radioisotope much higher than those used in commercial radioassays and, therefore, the sensitivity was sufficient to detect increases in serum TK1 in subjects with solid tumors.
Later, more sensitive, non-radioactive techniques enabled the lower increases from solid tumors to be measured accurately.
One major reason why the mortality is higher than the incidence is that lung cancer is mostly detected and diagnosed at a late stage.
[72][73][74][75][76] For diagnosis, combination of TK1 immunoassay with other biomarkers may be especially valuable[77] while falls in TK1 concentration following therapy may provide prognostic information.
The reason for this difference is the advances during the last decennia in the treatment of breast cancer cases and, above all, the public awareness that has allowed earlier diagnosis.
[37][79][80][81][82][83][84] Immunoassays may be more sensitive than enzyme activity assays for detecting the TK1 forms found in the serum of subjects with breast cancer.
Thymidine kinase has been suggested as a supplement to PSA (prostate-specific antigen), the tumor marker most frequently used in prostate cancer.
[97] There are several non-malignant causes for elevation of thymidine kinase in serum including vitamin B12 deficiency, leading to pernicious anemia[98][99] viral infections (particularly by virus from the herpes group) [100][101][99] and wound healing after trauma and operation.
There are also reports of the use of thymidine kinase as a tumor marker in domestic animals, in horse,[102] in dogs[34][103][104][105][106][107] in cats[108] and in cows.
[114][115][116][117] Certain non-malignant diseases also give rise to dramatic elevation of TK values in cells and tissue: in peripheral lymphocytes during monocytosis[118] and in bone marrow during pernicious anemia.