Blood transfusion
Plasma is the "yellowish" liquid part of blood, which acts as a buffer and contains proteins and other important substances needed for the body's overall health.
[5][6][7] The administration of a single unit of blood is the standard for hospitalized people who are not bleeding, with this treatment followed with re-assessment and consideration of symptoms and hemoglobin concentration.
[5] The advisory caution to use blood transfusion only with more severe anemia is in part due to evidence that outcomes are worsened if larger amounts are given.
An antibody panel consists of commercially prepared group O red cell suspensions from donors that have been phenotyped for antigens that correspond to commonly encountered and clinically significant alloantibodies.
It is preferable for the laboratory to obtain a pre-transfusion sample in these cases so a type and screen can be performed to determine the actual blood group of the patient and to check for alloantibodies.
The system should include monitoring, identification, reporting, investigation and analysis of adverse events, near-misses, and reactions related to transfusion and manufacturing.
[32] Haemovigilance systems have been established in many countries with the objective of ensuring the safety of blood for transfusion, but their organisational set-up and operating principles can vary.
However, because of latent infection (the "window period" in which an individual is infectious, but has not had time to develop antibodies) many cases of HIV seropositive blood were missed.
As with HIV, this low rate has been attributed to the ability to screen for both antibodies as well as viral RNA nucleic acid testing in donor blood.
[49] There has been controversy about whether a given product unit's age is a factor in transfusion efficacy, specifically about whether "older" blood directly or indirectly increases risks of complications.
[80] Working at the Royal Society in the 1660s, the physician Richard Lower began examining the effects of changes in blood volume on circulatory function and developed methods for cross-circulatory study in animals, obviating clotting by closed arteriovenous connections.
The new instruments he was able to devise enabled him to perform the first reliably documented successful transfusion of blood in front of his distinguished colleagues from the Royal Society.
[citation needed] According to Lower's account, "...towards the end of February 1665 [I] selected one dog of medium size, opened its jugular vein, and drew off blood, until its strength was nearly gone.
[81] The first blood transfusion from animal to human was administered by Dr. Jean-Baptiste Denys, eminent physician to King Louis XIV of France, on June 15, 1667.
[citation needed] In the early 19th century, British obstetrician Dr. James Blundell made efforts to treat hemorrhage by transfusion of human blood using a syringe.
[89] In 1840, at St George's Hospital Medical School in London, Samuel Armstrong Lane, aided by Blundell, performed the first successful whole blood transfusion to treat haemophilia.
John Braxton Hicks was the first to experiment with chemical methods to prevent the coagulation of blood at St Mary's Hospital, London in the late-19th century.
[98][99] Their first report in March 1915 showed that gelatine, agar, blood serum extracts, starch and beef albumin proved to be useless preservatives.
"[105] In June 1915, they made a crucial report in the Journal of the American Medical Association that agglutination could be avoided if the blood samples of the donor and recipient were tested before.
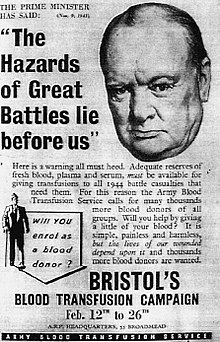
"[106] Canadian doctor and Lieutenant Lawrence Bruce Robertson became instrumental in persuading the Royal Army Medical Corps to adopt the use of blood transfusion at the Casualty Clearing Stations for the wounded.
[109] Oswald Hope Robertson, a medical researcher and U.S. Army officer, was attached to the RAMC in 1917, where he became instrumental in establishing the first blood banks in preparation for the anticipated Third Battle of Ypres.
[110] He used sodium citrate as the anticoagulant; blood was extracted from punctures in the vein and was stored in bottles at British and American Casualty Clearing Stations along the Front.
[108] Geoffrey Keynes, a British surgeon, developed a portable machine that could store blood to enable transfusions to be carried out more easily.
Similar systems developed in other cities, including Sheffield, Manchester and Norwich, and the service's work began to attract international attention.
Bogdanov was motivated, at least in part, by a search for eternal youth, and remarked with satisfaction on the improvement of his eyesight, suspension of balding, and other positive symptoms after receiving 11 transfusions of whole blood.
[113] Following Bogdanov's lead, Vladimir Shamov and Sergei Yudin in the USSR pioneered the transfusion of cadaveric blood from recently deceased donors.
[116] Frederic Durán-Jordà fled to Britain in 1938 and worked with Dr Janet Vaughan at the Royal Postgraduate Medical School at Hammersmith Hospital to establish a system of national blood banks in London.
[127] By 2013 the number had declined to about 11 million units, because of the shift towards laparoscopic surgery and other surgical advances and studies that have shown that many transfusions were unnecessary.
Non-blood volume expanders are available for cases where only volume restoration is required, but a substance with oxygen-carrying capacity would help doctors and surgeons avoid the risks of disease transmission and immune suppression, address the chronic blood donor shortage, and address the concerns of Jehovah's Witnesses and others who have religious objections to receiving transfused blood.
Hemopure, a hemoglobin-based therapy, is approved for use in South Africa and has been used in the United States on a case-by-case basis through the emergency Investigational New Drug (IND) process.