Trichomonas vaginalis
Trichomonas vaginalis is an anaerobic, flagellated protozoan parasite and the causative agent of a sexually transmitted disease called trichomoniasis.
[5] Alfred Francois Donné (1801–1878) was the first to describe a procedure to diagnose trichomoniasis through "the microscopic observation of motile protozoa in vaginal or cervical secretions" in 1836.
[9] Some of the complications of Trichomonas vaginalis in women include: preterm delivery, low birth weight, and increased mortality as well as predisposing to human immunodeficiency virus infection, AIDS, and cervical cancer.
[10] Trichomonas vaginalis can be seen in diverse locations within the body, such as," in the urinary tract, fallopian tubes, and pelvis and can cause pneumonia, bronchitis, and oral lesions.
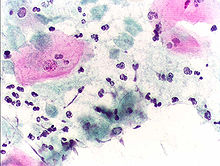
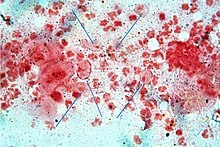
"[11] Classically, with a cervical smear, infected women may have a transparent "halo" around their superficial cell nucleus but more typically the organism itself is seen with a, "slight cyanophilic tinge, faint eccentric nuclei, and fine acidophilic granules.
[21] The nucleus is usually elongated, and is located near the anterior end of the protozoan within the cytoplasm which contains many hydrogenosomes (closed-membrane organelle with the ability to produce both adenosine triphosphate and hydrogen while in anaerobic conditions.
[27] There is an absence of cytochrome C and mitochondria, thus making oxygen uptake and synthesis of adenosine triphosphate via oxidative phosphorylation difficult.
[27] Although it contains no mitochondria, an analogous structure called a hydrogenosome, which is the site of fermentative oxidation of pyruvate, carries out many of the same metabolic processes.
Carbohydrates, specifically those with alpha1,4- glycosidic linkages, are metabolized and eventually fermented to produce products such as acetate, lactate, malate, glycerol and CO2 under aerobic conditions.
The amoeboid form, which is pancake shaped, allows for greater surface area contact with epithelial cells of the vagina, cervix, urethra, and prostate.
The adhesins are four trichomonad enzymes called AP65, AP51, AP33, and AP23 that mediate the interaction of the parasite to the receptor molecules on vaginal epithelial cells.
[29] This molecule is the most abundant on the surface of Trichomonas vaginalis, aids in sticking to vaginal epithelial cells, and can also influence how the human immune system responds, affecting inflammatory responses and macrophages in the body.
[34]) As much as two-thirds of the Trichomonas vaginalis sequence consists of repetitive and transposable elements, indicative of a recent drastic, evolutionarily expansion of the genome.
[36] High levels of genetic diversity were detected in Trichomonas vaginalis after phenotypic differences were discovered during clinical presentations.
Trichomonas vaginalis virus infection is clinically relevant in that, it has an effect on parasite resistance to metronidazole, a first line drug treatment for human trichomoniasis.
Having Trichomonas vaginalis also may increase the chances of the infected woman transmitting human immunodeficiency virus to her sexual partner(s).