Ulegyria
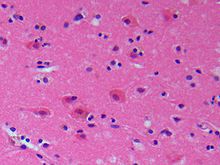
Ulegyria is a diagnosis used to describe a specific type of cortical scarring in the deep regions of the sulcus that leads to distortion of the gyri.
[3] Overall, the physical structure of affected areas in the brain is described as a “mushroom”-like shape in which the gyri are unusually large and the sulci become wider deeper in the cortex.
[1] This mushroom-like structure is the result of the lower parts of the ulegyria-affected area being more prone to deterioration, while the upper gyri are usually spared.
[2][9] Ulegyria develops as a result of a brain injury called cerebral ischemia surrounding the time of an infant's birth.
Oftentimes, fetal hypoxic-ischemic brain injuries occur as a result of a pregnancy complications such as placental abruption, cord accident, or cardiovascular stress due to a difficult delivery.
If sympathetic nervous system activation does not produce any improvement, oxygen levels will continue to fall and disruptions to metabolism, other cellular processes, and overall functioning will ensue.
Continued influx of calcium serves to constitutively activate downstream effectors, including lipases, proteases, and endonucleases, whose actions eventually destroy the cell skeleton.
Protein synthesis all over the body is severely inhibited and essentially comes to a standstill while the brain is suffering from acute oxygen deprivation.
Areas particularly vulnerable to the damaging effects of hypoxic episodes include: the superior brainstem, the cerebellum, white matter and subcortical structures supplied by the branches of deep and superficial penetrating blood vessels.
It has been hypothesized that because pre-term babies don't have fully developed sympathetic nervous systems, they cannot react as well to low oxygen saturation levels caused by the cerebral hemorrhage.
Recent research has found a connection between intrauterine infections and inflammation in the mother and an increased likelihood of perinatal brain damage in the fetus.
This study suggested that intrauterine infections in the mother could affect glial cells and toll-like receptors (TLRs) which are important in moderating the inflammatory response in the fetal brain.
This form of the disease involves symptoms that would be expected from damage to the parietal and occipital lobes: seizures with visual hallucinations, visuospatial dysfunction, tingling, numbness, pain, and a burning sensation.
[7] Polymicrogyria is characterized by excessive folding of the surface gyri and a thickening of the cerebral cortex,[18] rather than the sulcal scarring that is typical of ulegyria.
An MRI image of ulegyria is identified by mushroom shaped gyri, deformities in white matter, and localization mainly in the posterior cerebral region.
In addition, unaffected gyri are also present in especially bilateral watershed regions indicating delayed effects of perinatal hypoxic damage.
[7] For example, when EEG tests in epileptic patients show deviations in the frontal and central-parietal regions, ulegyria can be considered to be present in that area.
For instance, seizures caused by epilepsy, due to the presence of ulegyria in the occipital lobe, can be controlled using antiepileptic drugs in some patients.
[1] In other patients, such as those who suffer from ulegyria in the posterior cortex, drugs are not effective and surgery of the area causing epilepsy is needed.