Riboflavin
Natural sources of riboflavin include meat, fish and fowl, eggs, dairy products, green vegetables, mushrooms, and almonds.
Industrial synthesis of riboflavin was initially achieved using a chemical process, but current commercial manufacturing relies on fermentation methods using strains of fungi and genetically modified bacteria.
FAD is the more abundant form of flavin, reported to bind to 75% of the number of flavin-dependent protein encoded genes in the all-species genome (the flavoproteome)[6][7] and serves as a co-enzyme for 84% of human-encoded flavoproteins.
The flavin coenzymes support the function of roughly 70-80 flavoenzymes in humans (and hundreds more across all organisms, including those encoded by archeal, bacterial and fungal genomes) that are responsible for one- or two-electron redox reactions which capitalize on the ability of flavins to be converted between oxidized, half-reduced and fully reduced forms.
[4] An enzyme involved in folate metabolism, 5,10-methylenetetrahydrofolate reductase, requires FAD to form the amino acid, methionine, from homocysteine.
[4] Riboflavin deficiency appears to impair the metabolism of the dietary mineral, iron, which is essential to the production of hemoglobin and red blood cells.
[18] In the presence of high concentrations of hydrocarbons or aromatic compounds, some bacteria overproduce riboflavin, possibly as a protective mechanism.
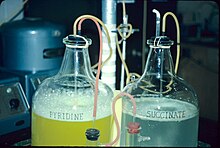
One such organism is Micrococcus luteus (American Type Culture Collection strain number ATCC 49442), which develops a yellow color due to production of riboflavin while growing on pyridine, but not when grown on other substrates, such as succinic acid.
[18][19] A substituted aniline, produced by reductive amination using D-ribose, was condensed with alloxan in the final step: Keratoconus is the most common form of corneal ectasia, a progressive thinning of the cornea.
[23] A 2017 review reported that daily riboflavin taken at 400 mg per day for at least three months may reduce the frequency of migraine headaches in adults.
[26] The National Academy of Medicine updated the Estimated Average Requirements (EARs) and Recommended Dietary Allowances (RDAs) for riboflavin in 1998.
As for safety, the IOM sets tolerable upper intake levels (ULs) for vitamins and minerals when evidence is sufficient.
[28][29] The EFSA also considered the maximum safe intake and like the U.S. National Academy of Medicine, decided that there was not sufficient information to set an UL.
[24] For U.S. food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of Daily Value (%DV).
[31] With normal dietary intake, about two-thirds of urinary output is riboflavin, the remainder having been partially metabolized to hydroxymethylriboflavin from oxidation within cells, and as other metabolites.
When consumption exceeds the ability to absorb, riboflavin passes into the large intestine, where it is catabolized by bacteria to various metabolites that can be detected in feces.
[44] Riboflavin deficiency is uncommon in the United States and in other countries with wheat flour or corn meal fortification programs.
[39] From data collected in biannual surveys of the U.S. population, for ages 20 and over, 22% of women and 19% of men reported consuming a supplement that contained riboflavin, typically a vitamin-mineral multi-supplement.
[3] A deficiency of riboflavin can be primary (i.e. caused by poor vitamin sources in the regular diet) or secondary, which may be a result of conditions that affect absorption in the intestine.
[42][51] Infants and young children present with muscle weakness, cranial nerve deficits including hearing loss, sensory symptoms including sensory ataxia, feeding difficulties, and respiratory distress caused by a sensorimotor axonal neuropathy and cranial nerve pathology.
[42][51] Other inborn errors of metabolism include riboflavin-responsive multiple acyl-CoA dehydrogenase deficiency, also known as a subset of glutaric acidemia type 2, and the C677T variant of the methylenetetrahydrofolate reductase enzyme, which in adults has been associated with risk of high blood pressure.
[3][52] Riboflavin excretion rates decrease as a person ages, but increase during periods of chronic stress and the use of some prescription drugs.
[4][5] The erythrocyte glutathione reductase activity coefficient (EGRAC) provides a measure of tissue saturation and long-term riboflavin status.
In 1879, Blyth isolated a water-soluble component of cows' milk whey, which he named "lactochrome", that fluoresced yellow-green when exposed to light.
The confusion was due to the fact that riboflavin (B2) deficiency causes stomatitis symptoms similar to those seen in pellagra, but without the widespread peripheral skin lesions.
[54] In 1935, Paul Gyorgy, in collaboration with chemist Richard Kuhn and physician T. Wagner-Jauregg, reported that rats kept on a B2-free diet were unable to gain weight.
[55] Isolation of B2 from yeast revealed the presence of a bright yellow-green fluorescent product that restored normal growth when fed to rats.
This observation enabled the researchers to develop a rapid chemical bioassay in 1933, and then isolate the factor from egg white, calling it ovoflavin.
In 1934, Kuhn's group identified the chemical structure of these flavins as identical, settled on "riboflavin" as a name, and were also able to synthesize the vitamin.
[57] In 1939, it was confirmed that riboflavin is essential for human health through a clinical trial conducted by William H. Sebrell and Roy E. Butler.