Cervical cancer
[16][17] Minor risk factors include smoking, a weak immune system, birth control pills, starting sex at a young age, and having many sexual partners.
[32] Expected scenarios for the reduction of mortality due to cervical cancer worldwide (and specially in low-income countries) have been reviewed, given assumptions with respect to the achievement of recommended prevention targets using triple-intervention strategies defined by WHO.
[35] The date marks the day in 2020 when WHO launched the Global strategy to accelerate the elimination of cervical cancer as a public health problem, with a resolution passed by 194 countries.
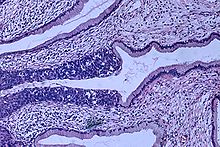
The World Health Organization classification system was descriptive of the lesions, naming them mild, moderate, or severe dysplasia or carcinoma in situ (CIS).
[68][69] The term cervical intraepithelial neoplasia (CIN) was developed to place emphasis on the spectrum of abnormality in these lesions, and to help standardize treatment.
[90] This is in part because many of these countries have an impoverished health care infrastructure, too few trained and skilled professionals to obtain and interpret Pap tests, uninformed women who get lost to follow-up, and a lengthy turn-around time to get results.
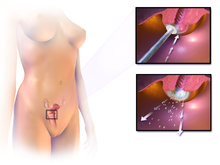
[95] The treatment of cervical cancer varies worldwide, largely due to access to surgeons skilled in radical pelvic surgery and the emergence of fertility-sparing therapy in developed nations.
Surgical techniques that remove more cervical tissue come with less risk of the cancer recurring but a higher chance of giving birth prematurely.
Due to this risk, taking into account the age, childbearing plans of the woman, and the size and location of the cancer cells are crucial for choosing the right procedure.
[102][103] A systematic review concluded that more evidence is needed to inform decisions about different surgical techniques for women with cervical cancer at stage IA2.
If the surgeon is not able to microscopically confirm clear margins of cervical tissue once the woman is under general anaesthesia in the operating room, a hysterectomy may still be needed.
[citation needed] Early stages (IB1 and IIA less than 4 cm) can be treated with radical hysterectomy with removal of the lymph nodes or radiation therapy.
Women treated with surgery who have high-risk features found on pathologic examination are given radiation therapy with or without chemotherapy to reduce the risk of relapse.
[citation needed] A Cochrane review has found moderate-certainty evidence that radiation decreases the risk of disease progression in people with stage IB cervical cancer when compared to no further treatment.
[114] Such addition of platinum-based chemotherapy to chemoradiation seems not only to improve survival but also reduces risk of recurrence in women with early-stage cervical cancer (IA2–IIA).
[118] There is insufficient evidence of whether anticancer drugs after standard care help women with locally advanced cervical cancer to live longer.
[121] A 2019 review found no controlled trials regarding the efficacy and safety of interventions for vaginal bleeding in women with advanced cervical cancer.
[122] Immunotherapy with immune checkpoint inhibitors, such as pembrolizumab (Keytruda), has also been approved by the U.S. Food and Drug Administration (FDA) for certain patients with recurrent or metastatic cervical cancer, demonstrating promising results in ongoing clinical trials.
[123] [124] In October 2021, the FDA expanded this approval to include pembrolizumab in combination with chemotherapy, with or without bevacizumab, for people with persistent, recurrent, or metastatic cervical cancer, underscoring the potential of immunotherapeutic approaches in this setting.
Another immune checkpoint inhibitor, cemiplimab-rwlc (Libtayo), received FDA approval in September 2022 for patients with recurrent or metastatic cervical cancer that has progressed on or after chemotherapy, further highlighting the expanding role of immunotherapeutic strategies in advanced disease.
Common acute RT effects involve the gastrointestinal system, e.g., diarrhea and constipation; urinary tract, e.g., frequent urination; and may cause cervicitis.
Common late RT complications include: infertility or premature ovarian failure; vaginal stenosis; lower motor neuron syndrome; telangiectasias, and subsequent hemorrhage; and progressive myelopathy, which may result in irreversible neurologic deficits ranging from minor sensory symptoms to complete paraplegia.
[138] Radiotherapy late effects (with occurrence rates) include osteonecrosis (8-20%), bladder ulceration (<3%), vaginal stenosis (>2.5%)[139] and chronic pelvic radiation disease (1-10%), e.g., irreversible lumbosacral plexopathy.
[146] Regular twice-yearly Pap tests can reduce the incidence of cervical cancer up to 90% in Australia, and save 1,200 Australian women from dying from the disease each year.
[152] As of 2022, the World Health Organization announced that "each year in the WHO European Region more than 66 000 women are newly diagnosed with cervical cancer and more than 30 000 die from this preventable disease.
[156] The annual direct medical cost of cervical cancer prevention and treatment before the introduction of the HPV vaccine was estimated at $6 billion.
In summary, HSV was seen as a likely cause because it is known to survive in the female reproductive tract, and to be transmitted sexually in a way compatible with known risk factors, such as promiscuity and low socioeconomic status.
[170] In 2006, the US Food and Drug Administration (FDA) approved the first preventive HPV vaccine, marketed by Merck & Co. under the trade name Gardasil.
[35] The date marks the day in 2020 when WHO launched the Global strategy to accelerate the elimination of cervical cancer as a public health problem, with a resolution passed by 194 countries.
[172] There are several factors that may limit indigenous women from engaging in regular cervical screening practices, including sensitivity in discussing the topic in Aboriginal communities, embarrassment, anxiety and fear about the procedure.







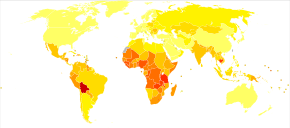
|
no data
<2.4
2.4–4.8
4.8–7.2
7.2–9.6
9.6–12
12–14.4
|
14.4–16.8
16.8–19.2
19.2–21.6
21.6–24
24–26.4
>26.4
|
