Deep vein thrombosis
[1] The most common life-threatening concern with DVT is the potential for a clot to embolize (detach from the veins), travel as an embolus through the right side of the heart, and become lodged in a pulmonary artery that supplies blood to the lungs.
[12] The most frequent long-term DVT complication is post-thrombotic syndrome, which can cause pain, swelling, a sensation of heaviness, itching, and in severe cases, ulcers.
[13] Risk factors include recent surgery, older age, active cancer, obesity, infection, inflammatory diseases, antiphospholipid syndrome, personal history and family history of VTE, trauma, injuries, lack of movement, hormonal birth control, pregnancy, and the period following birth.
[12] When not fatal, PE can cause symptoms such as sudden onset shortness of breath or chest pain, coughing up blood (hemoptysis), and fainting (syncope).
[20] Symptoms concerning for DVT are more often due to other causes, including cellulitis, ruptured Baker's cyst, hematoma, lymphedema, and chronic venous insufficiency.
[56] Inactivity and immobilization contribute to venous stasis, as with orthopedic casts,[65] paralysis, sitting, long-haul travel, bed rest, hospitalization,[62] catatonia,[66] and in survivors of acute stroke.
Oral contraceptives[b] and hormonal replacement therapy increase the risk through a variety of mechanisms, including altered blood coagulation protein levels and reduced fibrinolysis.
[14] Additionally, approximately 5% of people have been identified with a background genetic risk comparable to the factor V Leiden and prothrombin G20210A mutations.
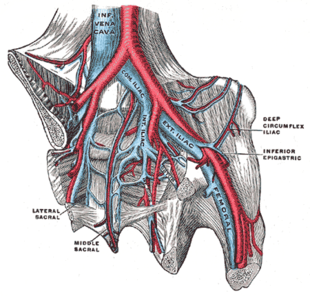
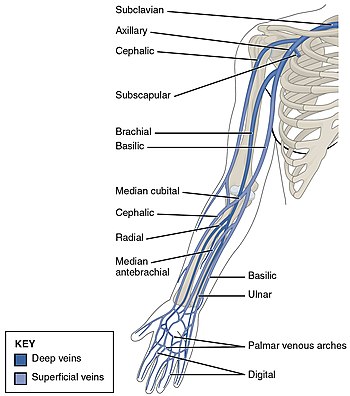
[101] Common risk factors for having an upper extremity DVT include having an existing foreign body (such as a central venous catheter, a pacemaker, or a triple-lumen PICC line), cancer, and recent surgery.
[62] The beginning of venous thrombosis is thought to arise from "activation of endothelial cells, platelets, and leukocytes, with initiation of inflammation and formation of microparticles that trigger the coagulation system" via tissue factor.
[55] They release pro-coagulant granules[109] and neutrophil extracellular traps (NETs) or their components, which play a role in venous thrombi formation.
[84] Cancer also produces unique substances that stimulate factor Xa, cytokines that promote endothelial dysfunction, and plasminogen activator inhibitor-1, which inhibits the breakdown of clots (fibrinolysis).
Hypoxemia also results in the production of reactive oxygen species, which can activate these pathways, as well as nuclear factor-κB, which regulates hypoxia-inducible factor-1 transcription.
[114] A clinical probability assessment using the Wells score (see column in the table below) to determine if a potential DVT is "likely" or "unlikely" is typically the first step of the diagnostic process.
The score is used in suspected first lower extremity DVT (without any PE symptoms) in primary care and outpatient settings, including the emergency department.
[1] Compression ultrasonography for suspected deep vein thrombosis is the standard diagnostic method, and it is highly sensitive for detecting an initial DVT.
[1] A thorough clinical assessment is needed and should include a physical examination, a review of medical history, and universal cancer screening done in people of that age.
[5][142] Drawbacks of catheter-directed thrombolysis (the preferred method of administering the clot-busting enzyme[5]) include a risk of bleeding, complexity,[l] and the cost of the procedure.
[125] In 2020, NICE kept their 2012 recommendations that catheter-directed thrombolysis should be considered in those with iliofemoral DVT who have "symptoms lasting less than 14 days, good functional status, a life expectancy of 1 year or more, and a low risk of bleeding.
[143] Catheter-directed thrombolysis with thrombectomy[141] against iliofemoral DVT has been associated with a reduction in the severity of post-thrombotic syndrome at an estimated cost-effectiveness ratio of about $138,000[m] per gained QALY.
This treatment involves initial anticoagulation followed by thrombolysis of the subclavian vein and staged first rib resection to relieve the thoracic outlet compression and prevent recurrent DVT.
[150] Interventional radiology is the specialty that typically places and retrieves IVC filters,[151] and vascular surgery might do catheter directed thrombosis for some severe DVTs.
[156] Acutely ill hospitalized patients are suggested to receive a parenteral anticoagulant, although the potential net benefit is uncertain.
[63] DVT is most frequently a disease of older age that occurs in the context of nursing homes, hospitals, and active cancer.
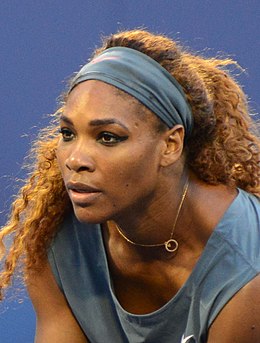
After feeling the sudden onset of a PE symptom, shortness of breath, she told her nurse and requested a CT scan and an IV heparin drip, all while gasping for air.
She started to receive an ultrasound to look for DVT in the legs, prompting her to express dissatisfaction to the medical staff that they were not looking for clots where she had symptoms (her lungs), and they were not yet treating her presumed PE.
[181] Dick Cheney was diagnosed with an episode while Vice President,[182] and TV show host Regis Philbin had DVT after hip-replacement surgery.
[187][188] In 1856, German physician and pathologist Rudolf Virchow published his analysis after the insertion of foreign bodies into the jugular veins of dogs, which migrated to the pulmonary arteries.
[120] Diagnoses were commonly performed by impedance plethysmography in the 1970s and 1980s,[191] but ultrasound, particularly after utility of probe compression was demonstrated in 1986, became the preferred diagnostic method.
[14] In their updated 2018 clinical practice guidelines, the American Society of Hematology identified 29 separate research priorities, most of which related to patients who are acutely or critically ill.[63] Inhibition of factor XI, P-selectin, E-selectin, and a reduction in formation of neutrophil extracellular traps are potential therapies that might treat VTE without increasing bleeding risk.