Essential hypertension
[6] Resistant hypertension is defined as the failure to reduce blood pressure to normal levels following an adequate trial of three antihypertensive medications.
[8] In single variant tests, it has been shown that SNPs were enriched for variants associated with adiposity, type 2 diabetes, coronary heart disease and kidney function in previously published GWAS, providing evidence that genetic loci related to blood pressure contribute to cardiovascular outcomes.
The majority of these studies support the concept that the inheritance is probably multifactorial or that a number of different genetic defects each has an elevated blood pressure as one of its phenotypic expressions.
It is believed that linking hypertension-related phenotypes with specific variations of the genome may yield definitive evidence of heritability.
It is argued there are numerous racial inequities, often inconspicuous, that contribute to black individuals having higher prevalence of essential hypertension than white people.
Access to social, financial, and educational resources that can enhance one's health is unequally impacted by racial prejudice.
There is experimental evidence that suggests that renal microvascular disease is an important mechanism for inducing salt-sensitive hypertension.
Renin is an enzyme secreted by the juxtaglomerular apparatus of the kidney and indirectly stimulates the release of aldosterone .
Insulin is a polypeptide hormone secreted by cells in the islets of Langerhans, which are contained throughout the pancreas.
Its main purpose is to regulate the levels of glucose in the body antagonistically with glucagon through negative feedback loops.
[29] Smoking directly causes a temporary increase in blood pressure through activation of the sympathetic nervous system by nicotine.
[31] It has been observed that individuals with a vitamin D deficiency have higher systolic and diastolic blood pressures than average.
Vitamin D inhibits renin secretion and its activity, it therefore acts as a "negative endocrine regulator of the renin–angiotensin system".
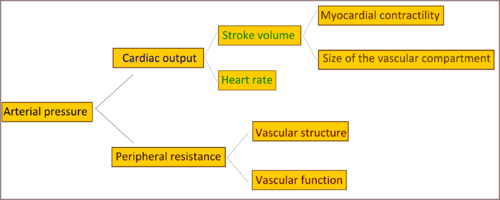
The pathophysiology of essential hypertension is an area of research, and until now remains not well understood, but many theories have been proposed to explain this.
The health care provider also may ask the patient to check readings at home or at other locations that have blood pressure equipment and to keep a written log of results.
The health care provider usually takes 2–3 readings at several medical appointments to diagnose high blood pressure.
[40] Prior to the work of Australian cardiovascular physiologist Paul Korner, in the 1940s, little was known about essential hypertension.