Glioblastoma
[2] Uncommon risk factors include genetic disorders, such as neurofibromatosis and Li–Fraumeni syndrome, and previous radiation therapy.
Common symptoms include seizures, headaches, nausea and vomiting, memory loss, changes to personality, mood or concentration, and localized neurological problems.
The tumor can start producing symptoms quickly, but occasionally is an asymptomatic condition until it reaches an enormous size.
[29] Similarly, exposure to formaldehyde, and residential electromagnetic fields, such as from cell phones and electrical wiring within homes, have been studied as risk factors.
Once cancerous, these cells are predisposed to spread along existing paths in the brain, typically along white-matter tracts, blood vessels and the perivascular space.
[34] The tumor may extend into the meninges or ventricular wall, leading to high protein content in the cerebrospinal fluid (CSF) (> 100 mg/dl), as well as an occasional pleocytosis of 10 to 100 cells, mostly lymphocytes.
Malignant cells carried in the CSF may spread (rarely) to the spinal cord or cause meningeal gliomatosis.
Tumors of this type usually arise from the cerebrum and may exhibit the classic infiltration across the corpus callosum, producing a butterfly (bilateral) glioma.
[35] Brain tumor classification has been traditionally based on histopathology at macroscopic level, measured in hematoxylin-eosin sections.
This update eliminated the classification of secondary glioblastoma and reclassified those tumors as Astrocytoma, IDH mutant, grade 4.
Their presence, coupled with the glioblastoma's diffuse nature results in difficulty in removing them completely by surgery, and is therefore believed to be the possible cause behind resistance to conventional treatments, and the high recurrence rate.
[54] Glioblastoma cancer stem cells appear to exhibit enhanced resistance to radiotherapy and chemotherapy mediated, at least in part, by up-regulation of the DNA damage response.
This is helpful in their extremely aggressive invasive behavior because quick adaptations in cellular volume can facilitate movement through the sinuous extracellular matrix of the brain.
[56] As of 2012, RNA interference, usually microRNA, was under investigation in tissue culture, pathology specimens, and preclinical animal models of glioblastoma.
[57] Additionally, experimental observations suggest that microRNA-451 is a key regulator of LKB1/AMPK signaling in cultured glioma cells[58] and that miRNA clustering controls epigenetic pathways in the disease.
[60] The high permeability and poor perfusion of the vasculature result in a disorganized blood flow within the tumor and can lead to increased hypoxia, which in turn facilitates cancer progression by promoting processes such as immunosuppression.
[63] Definitive diagnosis of a suspected GBM on CT or MRI requires a stereotactic biopsy or a craniotomy with tumor resection and pathologic confirmation.
Imaging of tumor blood flow using perfusion MRI and measuring tumor metabolite concentration with MR spectroscopy may add diagnostic value to standard MRI in select cases by showing increased relative cerebral blood volume and increased choline peak, respectively, but pathology remains the gold standard for diagnosis and molecular characterization.
Thus, IDH1 and IDH2 mutations are a useful tool to distinguish glioblastomas from astrocytomas, since histopathologically they are similar and the distinction without molecular biomarkers is unreliable.
[62] In all other instances of diffuse gliomas, a lack of IDH1 R132H immunopositivity should be followed by IDH1 and IDH2 DNA sequencing to detect or exclude the presence of non-canonical mutations.
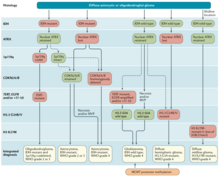
[66] Treating glioblastoma is difficult due to several complicating factors:[67] Treatment of primary brain tumors consists of palliative (symptomatic) care and therapies intended to improve survival.
Benefits of surgery include resection for a pathological diagnosis, alleviation of symptoms related to mass effect, and potentially removing disease before secondary resistance to radiotherapy and chemotherapy occurs.
[70] The chances of near-complete initial removal of the tumor may be increased if the surgery is guided by a fluorescent dye known as 5-aminolevulinic acid.
Other modalities, typically radiation and chemotherapy, are used after surgery in an effort to suppress and slow recurrent disease through damaging the DNA of rapidly proliferative GBM cells.
[73] Between 60-85% of glioblastoma patients report cancer-related cognitive impairments following surgery, which refers to problems with executive functioning, verbal fluency, attention, and speed of processing.
[89] In elderly people with newly diagnosed glioblastoma who are reasonably fit, concurrent and adjuvant chemoradiotherapy gives the best overall survival but is associated with a greater risk of haematological adverse events than radiotherapy alone.
[103] A good initial Karnofsky performance score (KPS) and MGMT methylation are associated with longer survival.
PPT refers to polyetherimide, PEG and trans-activator of transcription, and TRAIL is the human tumor necrosis factor-related apoptosis-induced ligand[114]) for effective gene delivery and tracking, with positive results.
Using new, more efficient delivery vectors and suicide gene-prodrug systems could improve the clinical benefit from these types of therapies.
[118][119] A clinical phase-I/II study with glioblastoma patients in Brazil investigated the natural compound perillyl alcohol for intranasal delivery as an aerosol.