Arrhythmia
[6] Those who have severe symptoms from an arrhythmia or are medically unstable may receive urgent treatment with a controlled electric shock in the form of cardioversion or defibrillation.
They are the most common causes of bradycardia:[citation needed] First, second, and third-degree blocks also can occur at the level of the sinoatrial junction.
There are many inherited conditions and heart diseases that can affect young people which can subsequently cause sudden death without advance symptoms.
[citation needed] If an arrhythmia results in a heartbeat that is too fast, too slow, or too weak to supply the body's needs, this manifests as lower blood pressure and may cause lightheadedness, dizziness, syncope, loss of consciousness, coma, persistent vegetative state, or brain death due to insufficient supply of blood and oxygen to the brain.
The first of arrhythmia is a result of enhanced or abnormal impulse formation originating at the pacemaker or the His-Purkinje network.
[21] Cardiac arrhythmia is often first detected by simple but nonspecific means: auscultation of the heartbeat with a stethoscope, or feeling for peripheral pulses.
These cannot usually diagnose specific arrhythmia but can give a general indication of the heart rate and whether it is regular or irregular.
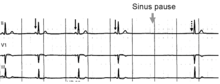
[citation needed] The simplest specific diagnostic test for assessment of heart rhythm is the electrocardiogram (abbreviated ECG or EKG).
[22][23] A Holter monitor is an EKG recorded over a 24-hour period, to detect arrhythmias that may happen briefly and unpredictably throughout the day.
Transesophageal atrial stimulation (TAS) instead uses an electrode inserted through the esophagus to a part where the distance to the posterior wall of the left atrium is only approximately 5–6 mm (remaining constant in people of different age and weight).
The impulse then spreads through both ventricles via the bundle of His and the Purkinje fibers causing a synchronized contraction of the heart muscle and, thus, the pulse.
[citation needed] The term sinus arrhythmia[26] refers to a normal phenomenon of alternating mild acceleration and slowing of the heart rate that occurs with breathing in and out respectively.
[citation needed] In adults and children over 15, resting heart rate faster than 100 beats per minute is labeled tachycardia.
Other conditions that increase sympathetic nervous system activity in the heart include ingested or injected substances, such as caffeine or amphetamines, and an overactive thyroid gland (hyperthyroidism) or anemia.
[citation needed] Any part of the heart that initiates an impulse without waiting for the sinoatrial node is called an ectopic focus and is, by definition, a pathological phenomenon.
This may cause a single premature beat now and then, or, if the ectopic focus fires more often than the sinoatrial node, it can produce a sustained abnormal rhythm.
Rhythms produced by an ectopic focus in the atria, or by the atrioventricular node, are the least dangerous dysrhythmias; but they can still produce a decrease in the heart's pumping efficiency because the signal reaches the various parts of the heart muscle with different timing than usual and can be responsible for poorly coordinated contraction.
[citation needed] Conditions that increase automaticity include sympathetic nervous system stimulation and hypoxia.
[31] When an entire chamber of the heart is involved in multiple micro-re-entry circuits and is, therefore, quivering with chaotic electrical impulses, it is said to be in fibrillation.
CPR can prolong the survival of the brain in the lack of a normal pulse, but defibrillation is the only intervention that can restore a healthy heart rhythm.
Defibrillation is performed by applying an electric shock to the heart, which resets the cells, permitting a normal beat to re-establish itself.
[citation needed] The method of cardiac rhythm management depends firstly on whether the affected person is stable or unstable.
[32] Several physical acts can increase parasympathetic nervous supply to the heart, resulting in blocking of electrical conduction through the AV node.
This can slow down or stop several arrhythmias that originate above or at the AV node (see main article: supraventricular tachycardias).
[citation needed] Some arrhythmias promote blood clotting within the heart and increase the risk of embolus and stroke.
Temporary pacing may be necessary for reversible causes of very slow heartbeats, or bradycardia (for example, from drug overdose or myocardial infarction).
In specialized catheter laboratories, they use fine probes inserted through the blood vessels to map electrical activity from within the heart.
This allows abnormal areas of conduction to be located very accurately and subsequently destroyed by heat, cold, electrical, or laser probes in a process called catheter ablation.
[34] Osborn waves on electrocardiogram (ECG) are frequent during targeted temperature management (TTM) after cardiac arrest, particularly in patients treated with 33 °C.
[35] Osborn waves are not associated with increased risk of ventricular arrhythmia, and may be considered a benign physiological phenomenon, associated with lower mortality in univariable analyses.