Pathophysiology of hypertension
[2][10][18][19] The autonomic nervous system plays a central role in maintaining cardiovascular homeostasis via pressure, volume, and chemoreceptor signals.
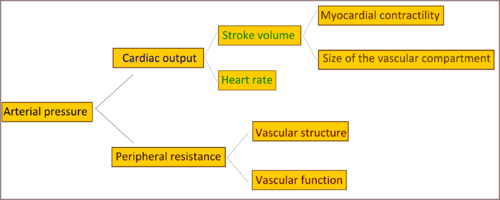
It does this by regulating the peripheral vasculature, and kidney function, which in turn affect cardiac output, vascular resistance, and fluid retention.
[20][21][22][23][24] The mechanisms of increased sympathetic nervous system activity in hypertension involve alterations in baroreflex and chemoreflex pathways at both peripheral and central levels.
[28][29][30] Additional small-molecule mediators that suppress baroreceptor activity and contribute to exaggerated sympathetic drive in hypertension include reactive oxygen species and endothelin.
[31][32] Some studies have shown that hypertensive patients manifest greater vasoconstrictor responses to infused norepinephrine than normotensive controls.
Renin is a circulating enzyme that participates in maintaining extracellular volume and arterial vasoconstriction, therefore contributing to regulation of blood pressure.
The activity of local renin–angiotensin systems and alternative pathways of angiotensin II formation may make an important contribution to remodeling of resistance vessels and the development of target organ damage (i.e. left ventricular hypertrophy, congestive heart failure, atherosclerosis, stroke, end-stage kidney disease, myocardial infarction, and arterial aneurysm) in hypertensive persons.
For example, local nitric oxide and endothelin, which are secreted by the endothelium, are the major regulators of vascular tone and blood pressure.
In patients with essential hypertension, the balance between the vasodilators and the vasoconstrictors is upset, which leads to changes in the endothelium and sets up a "vicious cycle" that contributes to the maintenance of high blood pressure.
[46][47][48] Normally nitric oxide is an important regulator and mediator of numerous processes in the nervous, immune and cardiovascular systems, including smooth muscle relaxation thus resulting in vasodilation of the artery and increasing blood flow, suppressor of migration and proliferation of vascular smooth-muscle cells.
The authors state that modern, western, high sodium, low potassium diets result in corresponding changes in intracellular concentration of these, the two most important cations in animal cells.
[55] Epidemiological support for this hypothesis can be found in a 2014 meta-analysis which states that "the sodium-to-potassium ratio appears to be more strongly associated with blood pressure outcomes than either sodium or potassium alone in hypertensive adult populations.".