Pelvic inflammatory disease
[1] Untreated PID can result in long-term complications including infertility, ectopic pregnancy, chronic pelvic pain, and cancer.
[2] However, in the UK it is reported by the NHS that infections by Neisseria gonorrhoeae and Chlamydia trachomatis are responsible for only a quarter of PID cases.
[2] It is recommended that the disease be considered in all women of childbearing age who have lower abdominal pain.
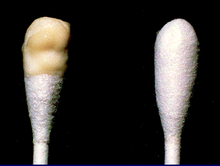
[2] A definitive diagnosis of PID is made by finding pus involving the fallopian tubes during surgery.
[11] In those with mild or moderate symptoms, a single injection of the antibiotic ceftriaxone along with two weeks of doxycycline and possibly metronidazole by mouth is recommended.
[12] A type of intrauterine device (IUD) known as the Dalkon shield led to increased rates of PID in the 1970s.
[2][1][13][14] Other complications include endometritis, salpingitis, tubo-ovarian abscess, pelvic peritonitis, periappendicitis, and perihepatitis.
[16] Occasionally, the infection can spread to the peritoneum causing inflammation and the formation of scar tissue on the external surface of the liver (Fitz-Hugh–Curtis syndrome).
N. gonorrhoeae has been isolated from fallopian tubes, facultative and anaerobic organisms were recovered from endometrial tissues.
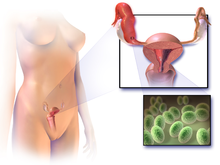
[19][20] The anatomical structure of the internal organs and tissues of the female reproductive tract provides a pathway for pathogens to ascend from the vagina to the pelvic cavity through the infundibulum.
The disturbance of the naturally occurring vaginal microbiota associated with bacterial vaginosis increases the risk of PID.
[19] PCR and serological tests have associated extremely fastidious organism with endometritis, PID, and tubal factor infertility.
In severe cases more testing may be required such as laparoscopy, intra-abdominal bacteria sampling and culturing, or tissue biopsy.
[23] Blood tests can also help identify the presence of infection: the erythrocyte sedimentation rate (ESR), the C-reactive protein (CRP) level, and chlamydial and gonococcal DNA probes.
[15] Definitive criteria include histopathologic evidence of endometritis, thickened filled fallopian tubes, or laparoscopic findings.
[25] Upon gynecologic ultrasound, a potential finding is tubo-ovarian complex, which is edematous and dilated pelvic structures as evidenced by vague margins, but without abscess formation.
[27] Acute pelvic inflammatory disease is highly unlikely when recent intercourse has not taken place or an IUD is not being used.
[citation needed] No single test has adequate sensitivity and specificity to diagnose pelvic inflammatory disease.
[41] This can be caused by the formation of scar tissue due to one or more episodes of PID, and can lead to tubal blockage.
[40] Certain occurrences such as a post pelvic operation, the period of time immediately after childbirth (postpartum), miscarriage or abortion increase the risk of acquiring another infection leading to PID.
[8]This is largely due to diagnostic tests being invasive and not included in routine check-ups, despite PID being the most common reason for individuals to admit themselves under gynecological care.
Despite the indications of a general decrease in PID rates, there is an observed rise in the prevalence of gonorrhea and chlamydia.