Portal hypertension
The signs and symptoms of both cirrhotic and non-cirrhotic portal hypertension are often similar depending on cause, with patients presenting with abdominal swelling due to ascites, vomiting of blood, and lab abnormalities such as elevated liver enzymes or low platelet counts.
[7] Complications include ascites, spontaneous bacterial peritonitis, variceal hemorrhage, hepatic encephalopathy, hepatorenal syndrome, and cardiomyopathy.
[12] Normally, SECs generate nitric oxide, which has several functions, including the maintenance of vascular tone and prevention of HSC activation.
Nitric oxide inhibition has been shown in some studies to increase portal hypertension and hepatic response to norepinephrine.
[13] Rising portal pressures leads to increased production of vasodilators, defective response to vasoconstrictors, and the formation of new blood vessels all within the splanchnic circulation.
To compensate for this low blood pressure, neurohumoral factors (RAAS, SNS, ADH) are activated, leading to sodium and water retention, and therefore, a high volume state.
Ultrasonography (US) is the first-line imaging technique for the diagnosis and follow-up of portal hypertension because it is non-invasive, low-cost and can be performed on-site.
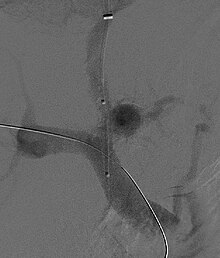
[17] The hepatic venous pressure gradient (HVPG) measurement has been accepted as the gold standard for assessing the severity of portal hypertension.
[20] The activation of neurohumoral factors as described in the "Pathophysiology" section results in a high volume state due to sodium and water retention.
The management of ascites needs to be gradual to avoid sudden changes in systemic volume status, which can precipitate hepatic encephalopathy, kidney failure, and death.
These bacteria (most commonly E. coli & Klebsiella) are able to pass through the intestinal wall and into ascitic fluid, leading to an inflammatory response.
[25][26] Both pharmacological (non-specific β-blockers, nitrate isosorbide mononitrate, vasopressin such as terlipressin) and endoscopic (banding ligation) treatment have similar results.
[27][28] The management of active variceal bleeding includes administering vasoactive drugs (somatostatin, octreotide), endoscopic banding ligation, balloon tamponade and TIPS.
[16] Eventually, the heart will no longer be able to maintain this increased cardiac output in the setting of prolonged splanchnic vasodilation.