Variant angina
Variant angina is caused by vasospasm, a narrowing of the coronary arteries due to contraction of the heart's smooth muscle tissue in the vessel walls.
[3] In comparison, stable angina is caused by the permanent occlusion of these vessels by atherosclerosis, which is the buildup of fatty plaque and hardening of the arteries.
Affected people usually have repeated episodes of unexplained (e.g., in the absence of exertion and occurring at sleep or in the early morning hours) chest pain, tightness in throat, chest pressure, light-headedness, excessive sweating, and/or reduced exercise tolerance that, unlike atherosclerosis-related angina, typically does not progress to myocardial infarction (heart attack).
Unlike cases of atherosclerosis-related stable angina, these symptoms are often unrelated to exertion and occur in night or early morning hours.
[4] However, individuals with atherosclerosis-related unstable angina may similarly exhibit night to early morning hour symptoms that are unrelated to exertion.
These agents include: In addition, hyperventilation and virtually any stressful emotional or physical (e.g. cold exposure) event that is suspected of causing significant rises in the blood levels of catecholamines may trigger variant angina.
However, the gold standard for diagnosing variant angina is to visualize coronary arteries by angiography before and after injection of a provocative agent such as ergonovine, methylergonovine or acetylcholine to precipitate an attack of vasospasm.
The onset of symptom relief in response to intravenous administration, which is used in more severe attacks of angina, occurs almost immediately while sublingual formulations of it act within 1–5 minutes.
Statins, e.g. fluvastatin, while not evaluated in large-scale double-blind studies, are reportedly helpful in reducing variant angina attacks and should be considered in patients when calcium channel blockers and nitroglycerin fail to achieve good results.
[4] There is also interest in using rho-kinase inhibitors, such as fasudil (available in Japan and China but not the USA),[16] and blocker of alpha-1 adrenergic receptors such as prazosin (which when activated cause vasodilation) but studies are needed to support their clinical utility in variant angina.
[4] Most individuals with variant angina have a favorable prognosis provided they are maintained on calcium channel blockers and/or long-acting nitrates; five-year survival rates in this group are estimated as over 90%.
[4][19] The Japanese Coronary Spasm Association established a clinical risk scoring system to predict outcomes for variant angina.
[20] Dr. William Heberden is credited with being the first to describe in a 1768 publication the occurrence of chest pain attacks (i.e. angina pectoris) that appeared due to pathologically occluded coronary arteries.
The disorder seems to occur more often in women than men, has a particularly high incidence in Japanese males as well as females, and affects individuals who may smoke tobacco products but exhibit few other cardiovascular risk factors.
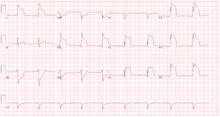
Finally, rare cases may exhibit symptom-free coronary artery spasm that is nonetheless associated with cardiac muscle ischemia (i.e. restricted blood flow and poor oxygenation) along with concurrent ischemic electrocardiographic changes.
For a portion of patients, variant angina may be a manifestation of a more generalized episodic smooth muscle-contractile disorder such as migraine, Raynaud's phenomenon, or aspirin-induced asthma.