Tertiary hyperparathyroidism
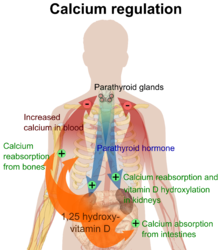
Persistent low levels of circulating calcium are thought to be the catalyst in the progressive development of adenoma, in the parathyroid glands resulting in primary hyperparathyroidism.
While primary hyperparathyroidism is the most common form of this condition,[2][3][4] secondary and tertiary are thought to result due to chronic kidney disease (CKD).
[6] Unlike primary hyperparathyroidism, the tertiary form presents as a progressive stage of resolved secondary hyperparathyroidism with biochemical hallmarks that include elevated calcium ion levels in the blood, hypercalcemia, along with autonomous production of parathyroid hormone and adenoma in all four parathyroid glands.
Further complications like secondary infections and necrosis can develop from this and can be fatal for some, making the monitoring of blood calcium and phosphate levels necessary.
[8][1] Conditions due to bone loss such as osteopenia and osteoporosis are common in tertiary hyperparathyroidism along with pathologic fractures.
Pseudoclubbing of the digits can also be indicative of a severe tertiary hyperparathyroidism due to excess resorption at the distal phalanges.
Radiological investigations include looking for signs of bone loss in both the hands and pelvis which is characteristic of tertiary hyperparathyroidism.
[8] Other clinical examination can include grading of muscle weakness, which is done by asking the patient to stand from a seated position with their hands folded across their chest.
Other common results from laboratory investigations would include decreased vitamin D levels, elevated blood parathyroid hormone and hyperphosphatemia.
[11] An elevated risk of developing tertiary hyperparathyroidism exists when late stage kidney disease is not corrected timely.
[18] Recurring tertiary hyperparathyroidism is generally seen to be caused by incomplete parathyroidectomy without renal transplant and the risk is increased when the parathyroid tissue left after surgery is that of a nodular type.
[23][4][8] Physiological changes due to the kidney damage adversely affect feedback loops that control secretion of parathyroid hormone.
[24] Primary hyperplasia, usually resulting in diffuse polyclonal growth is manly related to reversible secondary hyperparathyroidism.
Nodular hyperplastic glands in tertiary hyperparathyroidism are distinctly larger in both absolute size and weight up to 20-40-fold increases have been reported.
[27][14] Upon onset of hyperplasia these cells are described as having a nodular pattern with enlargement of protein synthesis machinery such as the endoplasmic reticulum and Golgi.
[7][2][1] Outcomes from surgery are generally favourable and a return to normalised blood calcium levels and parathyroid function is seen.
[1] In 1962, Dr C.E Dent reported that autonomous hyperparathyroidism may result from malabsorption syndromes and chronic kidney disease.
[6] The term 'tertiary hyperparathyroidism' was first used in 1963 by Dr Walter St. Gaur to describe a case reported on at Massachusetts General hospital.
[citation needed] It is now understood that tertiary hyperparathyroidism is defined as the presence of hypercalcemia, hyperphosphatemia and parathyroid hormone due to terminally biased parathyroid-bone-kidney feedback loop.