Hyperparathyroidism
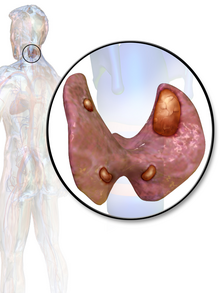
[2][3] In 80% of cases, primary hyperparathyroidism is due to a single benign tumor known as a parathyroid adenoma.
[2] Secondary hyperparathyroidism typically occurs due to vitamin D deficiency, chronic kidney disease, or other causes of low blood calcium.
[1] The diagnosis of primary hyperparathyroidism is made by finding elevated calcium and PTH in the blood.
[2] In patients with very high blood calcium levels, treatment may include large amounts of intravenous normal saline.
[1] While most primary patients are asymptomatic at the time of diagnosis, 'asymptomatic' is poorly defined and represents only those without "obvious clinical sequelae" such as kidney stones, bone disease, or hypercalcemic crisis.
[citation needed] In secondary hyperparathyroidism due to lack of vitamin D absorption, the parathyroid gland is behaving normally; clinical problems are due to bone resorption and manifest as bone syndromes such as rickets, osteomalacia, and renal osteodystrophy.
[20] The most common causes for secondary hyperparathyroidism include vitamin D deficiency, chronic kidney disease, inadequate calcium intake, malabsorption.
[24] The parathyroid glands separates from the pharyngeal wall and attaches to the posterior thyroid during the 7th week of human embryonic development.
[25] Alternatively, prolonged changes in serum calcium influences mRNA-binding proteins altering the encoding of PTH mRNA.
[26] There are also calcium independent mechanisms which include repression of PTH transcription through 1α,25-dihydroxyvitamin D binding with the vitamin D receptor.
[27] 3) PTH will also directly activate osteoclasts to cause bone resorption through degradation of hydroxyapatite and organic material.
Effects of PTH on the Kidneys Calcium reabsorption in the nephron occurs in proximal convoluted tubule and at the ascending Loop of Henle.
[28] PTH acts on the distal convoluted tubule and collecting duct to increase calcium reabsorption in the nephron.
The normal glands respond by secreting parathyroid hormone at a persistently high rate.
[30][31] Tertiary hyperparathyroidism has high serum calcium, phosphate, and PTH and low vitamin D levels.
[citation needed] Hyperparathyroidism can cause hyperchloremia and increase renal bicarbonate loss, which may result in a normal anion gap metabolic acidosis.
[33][34][35][36] Additionally a CT scan without contrast or renal ultrasound can be done to assess for nephrolithiasis and/or nephrocalcinosis if there is concern for it.
[36] Differential diagnoses of hypercalcemia include humoral hypercalcemia of malignancy, renal failure, malignant bone destruction (such as multiple myeloma, metastatic breast cancer, lymphoma), thiazide diuretics, lithium, immobilization, hyperthyroidism, milk alkali syndrome, multiple endocrine adenomatosis syndromes, and granulomatous diseases.
[42][43] In a minority of cases, this occurs as part of a multiple endocrine neoplasia (MEN) syndrome, either type 1 (caused by a mutation in the gene MEN1) or type 2a (caused by a mutation in the gene RET), which is also associated with the adrenal tumor pheochromocytoma.
[44][45] Patients with bipolar disorder who are receiving long-term lithium treatment are at increased risk for hyperparathyroidism.
However, only a few of these patients have significantly elevated levels of parathyroid hormone and clinical symptoms of hyperparathyroidism.
The bone disease in secondary hyperparathyroidism caused by kidney failure is termed renal osteodystrophy.
[50] Patients with late-stage kidney disease have an increased likelihood of developing tertiary hyperparathyroidism if not promptly corrected.
[51] In patients with late-stage kidney disease phosphate levels are elevated which directly affects the parathyroid glands and increases PTH production.
Additionally, it decrease the risk of nephrolithiasis, osteoporosis, fragility fractures, and improves bone mineral density.
While parathyroidectomy is recommended for all patients with hyperparathyroidism who are symptomatic, indications of surgery for those who are asymptomatic include the following:[53] A 2020 Cochrane systematic review compared the surgical procedures of minimally invasive parathyroidectomy and classically used bilateral neck exploration, however it did not find one approach to be superior to the other in either benefits or risks.
[citation needed] In patients with secondary hyperparathyroidism, the high PTH levels are an appropriate response to low calcium and treatment must be directed at the underlying cause of this (usually vitamin D deficiency or chronic kidney failure).
[57] A systematic review found surgical treatment to be superior regarding cure rates than medical therapy with cinacalcet with lower risk of complications.
[59][60] Treatment of secondary hyperparathyroidism with a calcimimetic in those on dialysis for CKD does not alter the risk of early death; however, it does decrease the likelihood of needing a parathyroidectomy.