Oral cancer
[16] The signs and symptoms of oral cancer depend on the location of the tumor but are generally thin, irregular, red and/or white patches in the mouth.
It can also be associated with loose teeth, bleeding gums, persistent ear ache, a feeling of numbness in the lip and chin, or swelling.
[25] The use of electronic cigarettes may also lead to the development of head and neck cancers due to the substances like propylene glycol, glycerol, nitrosamines, and metals contained therein, which can cause damage to the airways.
[30] The more alcohol is consumed regularly the higher the risk, but light to moderate drinking still somewhat increases the chances of getting oral cancer.
[33] As of 2024, there is some limited evidence supporting that the use of mouthwashes containing alcohol can increase the occurrence of oral cancer in some cases.
[35][34] In subgroup analyses, various combinations of smoking, drinking alcohol, poor oral hygiene, and using mouthwash several times a day for 35 years or more significantly increased risk.
[14] A 2023 meta-analysis observed that the HPV was present 6% of all oral cavity cancer cases, however without establishing a role of this virus in the oncogenesis of these tumors.
[39] Chewing betel quid (paan) and Areca nut-based products is known to be a strong risk factor for developing oral cancer even in the absence of tobacco.
Risk factors for developing HPV-positive oropharyngeal cancer include multiple sexual partners, anal and oral sex and a weak immune system.
[42] A premalignant (or precancerous) lesion is defined as "a benign, morphologically altered tissue that has a greater than normal risk of malignant transformation."
This ability is independent of the size or grade of the tumor (often seemingly slow growing cancers like the adenoid cystic carcinoma can metastasis widely).
[7] The full causal relation between alcohol consumption and the elevated risk of cancer remains unclear, but acetaldehyde plays a major role.
The acetaldehyde reacts with oral epithelial cells, inducing DNA modifications, which can lead to mutations and cancer development.
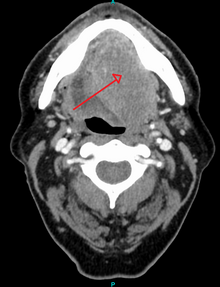
They may add additional information that can be used in staging, and treatment planning, such as the mitotic rate, the depth of invasion, and the HPV status of the tissue.
Panendoscopy may be recommended, because the tissues of the entire upper aerodigestive tract are generally affected by the same carcinogens, so other primary cancers are a common occurrence.
[52] TMN evaluation allows the person to be classified into a prognostic staging group;[52] The US Preventive Services Task Force (USPSTF) in 2013 stated evidence was insufficient to determine the balance of benefits and harms of screening for oral cancer in adults without symptoms by primary care providers.
[54] Micronuclei assays can help in early detection of pre-malignant and malignant lesions, thereby improving survival and reducing morbidity associated with treatment.
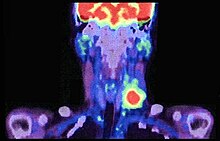
[55] Oral cancer (squamous cell carcinoma) is usually treated with surgery alone, or in combination with adjunctive therapy, including radiation, with or without chemotherapy.
[57] Chemotherapy and radiotherapy are most often used, as an adjunct to surgery, to control oral cancer that is greater than stage 1, or has spread to either regional lymph nodes or other parts of the body.
Overall, 2011 data from the SEER database shows that survival is around 57% at five years when all stages of initial diagnosis, all genders, all ethnicities, all age groups, and all treatment modalities are considered.
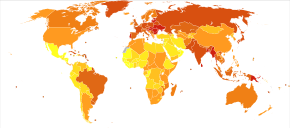
[62] Europe places second-highest after Southeast Asia among all continents for age-standardised rate (ASR) specific to oral and oropharyngeal cancer.
The same analysis applies to lifetime risk of developing oral cancer, as in Scotland it is 1.84% in males and 0.74% in females, higher than the rest of the UK, being 1.06% and 0.48%, respectively.
[65] The highest incidence of oral and pharyngeal cancer was recorded in Denmark, with age-standardised rates per 100,000 of 13.0, followed by Lithuania (9.9) and the United Kingdom (9.8).
[63] Incidence of oral cancer in young adults (ages 20–39 years old) in Scandinavia has reportedly risen approximately 6-fold between 1960 and 1994[66] The high incidence rate of oral and pharyngeal cancer in Denmark could be attributed to their higher alcohol intake than citizens of other Scandinavian countries and low intake of fruits and vegetables in general.
[67] Cigarette smoking, excessive alcohol consumption, inequalities in the care received by people with cancer, and gender-specific systemic risk factors have been determined as the leading causes for the high morbidity and mortality rates in Hungary.
In the previous year, 1.6% of lip and oral cavity cancers were diagnosed, where the age-standardised incidence rate (ASIR) across all geographic regions of United States of America estimates at 5.2 per 100,000 population.
[73] The ASIR across all geographic regions of South America as of 2012 sits at 3.8 per 100,000 population where approximately 6,046 deaths have occurred due to lip and oral cavity cancer, where the age-standardized mortality rate remains at 1.4.
Regionally incidence varies with highest rates in South Asia, particularly India, Bangladesh, Sri Lanka, Pakistan, and Afghanistan.
[75] In South East Asia and Arab countries, although the prevalence is not as high, estimated incidences of oral cancer ranged from 1.6 to 8.6/ 100,000 and 1.8 to 2.13/ 100,000 respectively.
[80] One of the reasons behind such high incidence might be popularity of betel and areca nuts, which are considered to be risk factors for development of oral cavity cancers.