Vertebral artery dissection
Over 75% recover completely or with minimal impact on functioning, with the remainder having more severe disability and a very small proportion (about 2%) dying from complications.
[1] It is suspected that VAD with headache as the only symptom is fairly common;[2] 8% of all cases of vertebral and carotid dissection are diagnosed on the basis of pain alone.
[1] Obstruction of blood flow through the affected vessel may lead to dysfunction of part of the brain supplied by the artery.
[1] In the event of involvement of the sympathetic tracts in the brainstem, a partial Horner's syndrome may develop; this is the combination of a drooping eyelid, constricted pupil, and an apparently sunken eye on one side of the face.
[3] The causes of vertebral artery dissection can be grouped under two main categories, spontaneous and traumatic.
[5] Marfan syndrome results from mutations in the FBN1 gene, defective production of the protein fibrillin-1, and a number of physical abnormalities including aneurysm of the aortic root.
[5] There have also been reports in other genetic conditions, such as osteogenesis imperfecta type 1, autosomal dominant polycystic kidney disease and pseudoxanthoma elasticum,[1] α1 antitrypsin deficiency and hereditary hemochromatosis, but evidence for these associations is weaker.
[7] Elevated homocysteine levels, often due to mutations in the MTHFR gene, appear to increase the risk of vertebral artery dissection.
[11] It has been difficult to prove the association of vertebral artery dissection with mild trauma and infections statistically.
These neurological events represent embolic phenomena due to loosening or breakdown of the clot at the site of the dissection, which can be triggered by low energy trauma or even occur spontaneously.
[15][16] A recent meta-analysis of the published data on the topic also looked to apply Hill's criteria for assigning causation in biological systems to the relationship between chiropractic adjustment and cervical artery dissection, finding that the relationship did not fulfill the required criteria for causality.
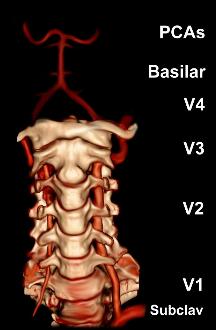
After exiting at the level of the first cervical vertebra, its course changes from vertical to horizontal, and then enters the skull through the foramen magnum.
In total, three quarters of the artery are outside the skull; it has a high mobility in this area due to rotational movement in the neck and is therefore vulnerable to trauma.
The vertebral artery supplies a number of vital structures in the posterior cranial fossa, such as the brainstem, the cerebellum and the occipital lobes.
[1][2] Various theories exist as to whether people who sustain carotid and vertebral artery dissection, even if they do not have a connective tissue disorder, have an underlying vulnerability.
Biopsy samples of skin and other arteries has indicated that this might be a possibility, but no genetic defect in collagen or elastin genes has been convincingly proven.
[1][3][17] Various diagnostic modalities exist to demonstrate blood flow or absence thereof in the vertebral arteries.
[1] Cerebral angiography is an invasive procedure, and it requires large volumes of radiocontrast that can cause complications such as kidney damage.
More rarely, thrombolysis (medication that dissolves blood clots) may be administered, and occasionally obstruction may be treated with angioplasty and stenting.
[1] From analysis of the existing small treatment trials of cervical artery dissection (carotid and vertebral) it appears that aspirin and anticoagulation (heparin followed by warfarin) are equally effective in reducing the risk of further stroke or death.
[3] Professional guidelines in the UK recommend that patients with VA dissection should be enrolled in a clinical trial comparing aspirin and anticoagulation if possible.
[21] Stenting involves the catheterization of the affected artery during angiography, and the insertion of a mesh-like tube; this is known as "endovascular therapy" (inside the blood vessel).
However, it is unclear whether the technical success of the procedure translates into improved outcomes, as in both cases the problem often resolves spontaneously over time.
[21] Stenting, as well as the insertion of coils by means of angiography, may be performed if there is an aneurysm and/or extension of the dissection into the V4 section of the artery.
[17] Surgery carries a high risk of complications, and is typically only offered in case of inexorable deterioration or contraindications to any of the other treatments.
The rate of survival with good outcome (a modified Rankin score of 0–2) is generally about 75%,[1][3] or possibly slightly better (85.7%) if antiplatelet drugs are used.
[1] Similarly, those living in urban areas are more likely to receive appropriate investigations, accounting for increased rates of diagnosis in those dwelling in cities.
In 1971, C. Miller Fisher, a Canadian neurologist and stroke physician working at Massachusetts General Hospital, first noted the "string sign" abnormality in carotid arteries on cerebral angiograms of stroke patients, and subsequently discovered that the same abnormality could occur in the vertebral arteries.
The short-pitched delivery bowled by NSW player Sean Abbott struck Hughes on the base of the skull, just behind his left ear which caused a vertebral artery dissection complicated by subarachnoid hemorrhage.