Arteriovenous malformation
Often the malformation is discovered as part of an autopsy or during treatment of an unrelated disorder (an "incidental finding"); in rare cases, its expansion or a micro-bleed from an AVM in the brain can cause epilepsy, neurological deficit, or pain.
[2] The most general symptoms of a cerebral AVM include headaches and epileptic seizures, with more specific symptoms that normally depend on its location and the individual, including:[1] Cerebral AVMs may present themselves in a number of different ways:[citation needed] Pulmonary arteriovenous malformations are abnormal communications between the veins and arteries of the pulmonary circulation, leading to a right-to-left blood shunt.
[citation needed] The anomaly can occur due to autosomal dominant diseases, such as hereditary hemorrhagic telangiectasia.
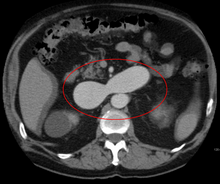
[9] An AVM interferes with this process by forming a direct connection of the arteries and veins, bypassing the capillary bed.
It can be extremely fragile and prone to bleeding because of the abnormally direct connections between high-pressure arteries and low-pressure veins.
[11] One indicator is a pulsing 'whoosh' sound caused by rapid blood flow through arteries and veins, which has been given the term bruit (French for 'noise').
[25] If a cerebral AVM is detected before a stroke occurs, usually the arteries feeding blood into the nidus can be closed off to avert the danger.