Dupuytren's contracture
[2] It is named after Guillaume Dupuytren, who first described the underlying mechanism of action, followed by the first successful operation in 1831 and publication of the results in The Lancet in 1834.
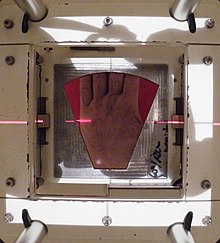
[6] It usually begins as small, hard nodules just under the skin of the palm,[2] then worsens over time until the fingers can no longer be fully straightened.
[4] Risk factors include family history, alcoholism, smoking, thyroid problems, liver disease, diabetes, previous hand trauma, and epilepsy.
[10] The Royal College of Radiologists (RCR) Faculty of Clinical Oncology concluded that radiotherapy is effective in early stage disease which has progressed within the last 6 to 12 months.
[citation needed] Dupuytren disease is generally considered painless, but can be painful if nerve tissue is involved, although this is not usually discussed in the literature.
The main function of the palmar fascia is to increase grip strength; thus, over time, Dupuytren's contracture decreases a person's ability to hold objects and use the hand in many different activities.
[19] Many risk factors have been suggested or identified: There may be three types of Dupuytren's disease:[31] Treatment is indicated when the so-called table-top test is positive.
[citation needed] The main categories listed by the International Dupuytren Society in order of stage of disease are radiation therapy, needle aponeurotomy (NA), collagenase injection, and hand surgery.
As of 2016[update] the evidence on the efficacy of radiation therapy was considered inadequate in quantity and quality, and difficult to interpret because of uncertainty about the natural history of Dupuytren's disease.
[34] Use of a splint to keep treated fingers straight following various forms of treatment, typically at all times for some days, then at nighttime for some weeks, is usual.
[35] On 12 June 1831, Dupuytren performed a surgical procedure on a person with contracture of the fourth and fifth digits who had been previously told by other surgeons that the only remedy was cutting the flexor tendons.
Because of high recurrence rates,[citation needed] new surgical techniques were introduced, such as fasciectomy and then dermofasciectomy.
[41][42][43] A 2015 Cochrane review reported that low-quality evidence suggested that fasciectomy may be more effective for people with advanced Dupuytren's contractures.
In most cases the graft is taken from the antecubital fossa (the crease of skin at the elbow joint) or the inner side of the upper arm.
[52] After this procedure the risk of recurrence is minimised,[42][52][53] but Dupuytren's can recur in the skin graft[54] and complications from surgery may occur.
After the excision and a careful hemostasis, the cellulose implant is placed in a single layer in between the remaining parts of the cord.
[62] The cord is then sectioned at as many levels as possible in the palm and fingers, depending on the location and extent of the disease, using perhaps a 25-gauge needle mounted on a 10 ml syringe.
[58] The advantage of needle aponeurotomy is the minimal intervention without incision (done in the office under local anesthesia) and the very rapid return to normal activities without need for rehabilitation, but the nodules may resume growing.
The tension on the cords is crucial, because tight constricting bands are most susceptible to be cut and torn by the small nicks, whereas the relatively loose neurovascular structures are spared.
[59] The cords are weakened through the injection of small amounts of the enzyme collagenase, which breaks peptide bonds in collagen.
[13] However, the Swedish manufacturer withdrew distribution of this drug in Europe[71] including the UK, Australia, and Asia in March 2020.
In a MCP joint contracture the needle must be placed at the point of maximum bowstringing of the palpable cord.
[60] After the injection the person's hand is wrapped in bulky gauze dressing and must be elevated for the rest of the day.
[60] After the treatment with collagenase the person should use a night splint and perform digital flexion/extension exercises several times per day for 4 months.
[10] The Royal College of Radiologists concluded that radiotherapy is effective in early stage disease which has progressed within the last 6 to 12 months.
"[76][77] Laser treatment (using red and infrared at low power) was informally discussed in 2013 at an International Dupuytren Society forum,[78] as of which time little or no formal evaluation of the techniques had been completed.
In 2021 improvement of Dupuytren's disease in a single patient by treatment with a fractionated CO₂ laser was reported.
[80] Besides hand therapy, many surgeons advise the use of static or dynamic splints after surgery to maintain finger mobility.
Cited disadvantages include joint stiffness, prolonged pain, discomfort,[82] subsequently reduced function and edema.
[83] A scoring system was made to evaluate the risk of recurrence and extension, based on the following values: bilateral hand involvement, little-finger surgery, early onset of disease, plantar fibrosis, knuckle pads, and radial side involvement.