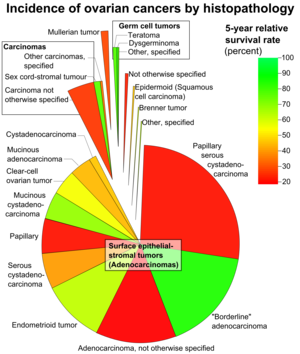
Surface epithelial-stromal tumor
Neoplasms in this group are thought to be derived from the ovarian surface epithelium (modified peritoneum) or from ectopic endometrial or fallopian tube (tubal) tissue.
While the 5-year survival rates of borderline tumors are excellent, this should not be seen as evidence of cure, as recurrences can occur many years later.
The appearance can look similar to colonic or ovarian cancer, but typically originates from the appendix (see mucinous adenocarcinoma with clinical condition Pseudomyxoma peritonei).
They are made of tubular glands bearing a close resemblance to benign or malignant endometrium.
Histologically, the tumor consists of nests of the aforementioned transitional cells within surrounding tissue that resembles normal ovary.
Small cell ovarian cancer (SCCO) are generally classified into epithelial tumors[16] associated with distinctive endocrine features.
[17] The World Health Organisation (WHO) recognises SCCO as two distinct entities: Small Cell Ovarian Cancer of Hypercalcemic Type (SCCOHT) and Small Cell Ovarian Cancer of Pulmonary Type (SCCOPT).
[20] There is also evidence to suggest that Pegylated Liposomal Doxorubicin with Carboplatin is tolerated better by people with platinum-sensitive relapsed EOC.
For surface epithelial-stromal tumors, the most common sites of metastasis are the pleural cavity (33%), the liver (26%), and the lungs (3%).
[23] On the other hand, in cases of conservative treatment in advanced stage borderline tumors, spontaneous pregnancy rates have been estimated to be 35% and the risk of lethal recurrence 2%.