Extracorporeal membrane oxygenation
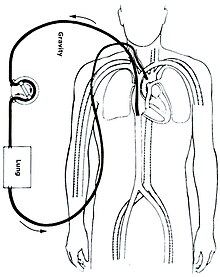
Extracorporeal membrane oxygenation (ECMO), is a form of extracorporeal life support, providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of oxygen, gas exchange or blood supply (perfusion) to sustain life.
The technology for ECMO is largely derived from cardiopulmonary bypass, which provides shorter-term support with arrested native circulation.
ECMO is also used to support patients with the acute viral pneumonia associated with COVID-19 in cases where artificial ventilation alone is not sufficient to sustain blood oxygenation levels.
Criteria for the initiation of ECMO vary by institution, but generally include acute severe cardiac or pulmonary failure that is potentially reversible and unresponsive to conventional management.
Examples of clinical situations that may prompt the initiation of ECMO include the following:[1] In those with cardiac arrest or cardiogenic shock, it is believed to improve survival and good outcomes.
[4] However, a recent clinical trial has shown that in patients with cardiogenic shock following acute myocardial infarction, ECLS did not improve survival (as measured via 30-day mortality); on the contrary, it resulted in increased complications (e.g., major bleeding, lower limb ischemia).
[5] This finding is corroborated by a recent meta-analysis [6] that used data from four previous clinical trials, indicating a need to reassess current guidelines for initiation of ECLS treatment.
[7] Initial reports indicated that it assisted in restoring patients' blood oxygen saturation and reducing fatalities among the approximately 3% of severe cases where it was utilized.
[8] For critically ill patients, the mortality rate reduced from around 59–71% with conventional therapy to approximately 46% with extracorporeal membrane oxygenation.
[9] A March 2021 Los Angeles Times cover story illustrated the efficacy of ECMO in an extremely challenging COVID patient.
[17][18][19] Even though ECMO is used for a range of conditions with varying mortality rates, early detection is key to prevent the progression of deterioration and increase survival outcomes.
A variety of complications can occur during cannulation, including vessel perforation with bleeding, arterial dissection, distal ischemia, and incorrect location.
[citation needed] Preterm infants, having inefficiency of the heart and lungs, are at unacceptably high risk for intraventricular hemorrhage (IVH) if ECMO is performed at a gestational age less than 32 weeks.
Other ECMO-specific factors predisposing to infections include the severity of illness in ECMO patients, the high risk of bacterial translocation from the gut and ECMO-related impairment of the immune system.
[26] Central VA ECMO may be used if cardiopulmonary bypass has already been established or emergency re-sternotomy has been performed (with cannulae in the right atrium (or SVC/IVC for tricuspid repair) and ascending aorta).
[27] Alternatively, a dual-lumen catheter is inserted into the right internal jugular vein, draining blood from the superior and inferior vena cavae and returning it to the right atrium.
Once it has been decided to inititiate ECMO, the patient is anticoagulated with intravenous heparin to prevent thrombus formation from clotting off the oxygenator.
[20]: 143 Cannulae can be placed percutaneously by the Seldinger technique, a relatively straightforward and common method for obtaining access to blood vessels, or via surgical cutdown.
Peripheral (femoral or jugular) cannulation can allow patients awaiting lung transplantation to remain awake and ambulatory with improved post-transplant outcomes.
[34][35] For those with respiratory failure, improvements in radiographic appearance, pulmonary compliance, and arterial oxyhemoglobin saturation indicate that the person may be ready to be taken off ECMO support.
For those with cardiac failure, enhanced aortic pulsatility correlates with improved left ventricular output and indicates that they may be ready to be taken off ECMO support.
[39] Lary commented on his initial work in a 2007 presentation wherein he writes, "Our research began by assembling an apparatus that, for the first time, kept animals alive while breathing pure nitrogen.
Shortly after its initial presentation to the American College of Surgeons, this apparatus was reviewed by Walton Lillehei who with DeWall made the first practical heart[–]lung machine that employed a bubble oxygenator.
2,857 (in 2023)[57] 129 (including rental units, in 2016)[59] Four randomized controlled trials (RCTs) have been conducted to evaluate the effectiveness of ECMO in respiratory failure patients.
The Conventional Ventilatory Support vs. Extracorporeal Membrane Oxygenation for Severe Adult Respiratory Failure (CESAR) Trial was a UK-based multicenter RCT aiming to evaluate the safety, efficacy and cost effectiveness of ECMO compared to conventional mechanical ventilation in adults with severe but reversible respiratory failure.
[65] The main conclusion the study authors drew from these results is that early ECMO initiation in severe ARDS patients does not provide a mortality benefit compared to continued standard of care treatment.