Fibrinogen
[1] Fibrin also mediates blood platelet and endothelial cell spreading, tissue fibroblast proliferation, capillary tube formation, and angiogenesis and thereby promotes revascularization and wound healing.
[1] Fibrinogen is a "positive" acute-phase protein, i.e. its blood levels rise in response to systemic inflammation, tissue injury, and certain other events.
The heximer is transferred to the Golgi where it is glycosylated, hydroxylated, sulfated, and phosphorylated to form the mature fibrinogen glycoprotein that is secreted into the blood.
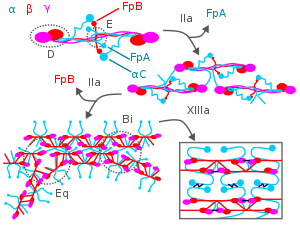
[10][12] Mature fibrinogen is arranged as a long flexible protein array of three nodules held together by a very thin thread which is estimated to have a diameter between 8 and 15 angstroms (Å).
The mutations have virtually complete genetic penetrance with essentially all homozygous bearers experiencing frequent and sometimes life-threatening episodes of bleeding and/or thrombosis.
Symptoms of the disorder, which more often occurs in individuals with lower plasma fibrinogen levels, include episodic bleeding and thrombosis that typically begin in late childhood or adulthood.
It is a form of congenital hypofibrinogenemia in which certain specific hereditary mutations in one copy of the FGG gene causes its fibrinogen product to accumulate in, and damage, liver cells.
[20] Hereditary fibrinogen Aα-Chain amyloidosis is an autosomal dominant extremely rare inherited disorder caused by a mutation in one of the two copies of the FGA gene.
It is a form of congenital dysfibrinogenemia in which certain mutations lead to the production of an abnormal fibrinogen that circulates in the blood while gradually accumulating in the kidney.
One well-studied cause of the disorder is severe liver disease including hepatoma, chronic active hepatitis, cirrhosis, and jaundice due to biliary tract obstruction.
The diseased liver synthesizes a fibrinogen which has a normally functional amino acid sequence but is incorrectly glycosylated (i.e. has a wrong amount of sugar residues) added to it during its passage through the Golgi.
Other, less well understood, causes are plasma cell dyscrasias and autoimmune disorders in which a circulating abnormal immunoglobulin or other protein interferes with fibrinogen function, and rare cases of cancer and medication (isotretinoin, glucocorticoids, and antileukemic drugs) toxicities.
In these cases, cryofibinogenema may or may not cause tissue injury and/or other symptoms and the actual cause-effect relationship between these diseases and the development of cryofibrinogenmia is unclear.
[23][24][25][26] Acquired hypofibrinogenemia is a deficiency in circulating fibrinogen due to excessive consumption that may occur as a result of trauma, certain phases of disseminated intravascular coagulation, and sepsis.
[27] Clinical analyses of the fibrinogen disorders typically measure blood clotting using the following successive steps:[28] Higher levels are, amongst others, associated with cardiovascular disease (>3.43 g/L).
[clarification needed] It may be elevated in any form of inflammation, as it is an acute-phase protein; for example, it is especially apparent in human gingival tissue during the initial phase of periodontal disease.
A particular pattern of migratory superficial vein thrombosis, termed trousseau's syndrome, occurs in, and may precede all other signs and symptoms of, these cancers.