Haemodynamic response
In haemodynamics, the body must respond to physical activities, external temperature, and other factors by homeostatically adjusting its blood flow to deliver nutrients such as oxygen and glucose to stressed tissues and allow them to function.
These cells control whether the vessels are constricted or dilated, which dictates the amount of oxygen and glucose that is able to reach the neuronal tissue.
These processes have the ability to take up various neurotransmitters, such as norepinephrine (NE) and glutamate, and perform various other functions to maintain chemical and electrical homeostasis in the neuronal environment.
When these calcium ion waves spread down the length of the astrocyte, phospholipase A (PLA2) is activated which in turn mobilizes arachidonic acid.
These two compounds are transported to the smooth muscle and there react with cytochrome P450 to make 20-hydroxyeicosatetraenoic acid (20-HETE), which acts through yet to-be-determined mechanisms to induce vasoconstriction.
[4] Dilation occurs when nitric oxide (NO) is released from endothelial cells and diffuses into nearby vascular smooth muscle.
It has also been proposed that NO may amplify astrocyte Ca2+ influx and activate Ca2+-dependent potassium channels, releasing K+ into the interstitial space and inducing hyperpolarization of smooth muscle cells.
[4] In addition to this, it has already been shown that NO stimulates increased cyclic GMP (cGMP) levels in the smooth muscle cells, inducing a signaling cascade that results in the activation of cGMP-dependent protein kinase (PKG) and an ultimate decrease in smooth muscle Ca2+ concentration.
Whether the vessels are constricted or dilated dictates the amount of oxygen and glucose that is able to reach the neuronal tissue.
A principal function of pericytes is to interact with astrocytes, smooth muscle cells, and other intracranial cells to form the blood brain barrier and to modulate the size of blood vessels to ensure proper delivery and distribution of oxygen and nutrients to neuronal tissues.
[7] These effects result from coagulation, which is normally prevented in the vascular endothelium by expression of antithrombotic factors on its surface.
Sepsis, which causes disruption and apoptosis of endothelial cells results in the endothelium switching to a procoagulant phenotype.
This includes pneumonia, parasitic infections, street drugs, such as cocaine and methamphetamines that cause constriction of blood vessels, and many more.
PAH deals with increase blood pressure in pulmonary arteries, which leads to shortness of breath, dizziness, fainting, rarely hemoptysis, and many other symptoms.
As a result of all of this, the left side of the heart has a hard time pumping a sufficient supply of oxygen to the rest of the body, which deteriorates the effect of the haemodynamic response.
Furthermore, there are no current cures for pulmonary arterial hypertension, but there are treatment options for patients with the disease to help prolong their survival and quality of life.
Moreover, high-dose calcium-channel blockers among patients who have a response to this treatment can prolong survival and improve pulmonary haemodynamics.
With a dysfunctional haemodynamic response, active neuronal tissue due to membrane depolarization lacks the necessary energy to propagate signals, as a result of blood flow hindrance.
In Alzheimer's disease, the fragments accumulate to form hard, insoluble plaques which reduce blood flow.
As a result, cellular energy failure, depolarization of neuronal and glial membranes, edema, and excess neurotransmitter and calcium ion release can occur.
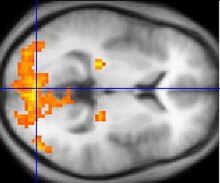
The measurement of haemodynamic response, in a clinical setting, can be used to create images of the brain in which especially active and inactive regions are shown as distinct from one another.
There are different fMRI techniques that can pick up a functional signal corresponding to changes in each of the previously mentioned components of the haemodynamic response.
The difference in magnetic properties of oxygenated and deoxygenated hemoglobin is what allows fMRI imaging to produce an effective map of which neurons are active and which are not.
Neuronal activity ultimately leads to an increase in local MR signaling corresponding to a decrease in the concentration of deoxyhemoglobin.
[15] Resting state fMRI enables the evaluation of the interaction of brain regions, when not performing a specific task.
[17] Before a PET scan begins, the patient will be injected with a small dose of a radioactive medicine tagged to a tracer such as glucose or oxygen.
PET scanners provide this feature because they measure the energy that is emitted when positrons from the radiotracer collide with electrons in the brain.