Malaria
[1] Methods that use the polymerase chain reaction to detect the parasite's DNA have been developed, but they are not widely used in areas where malaria is common, due to their cost and complexity.
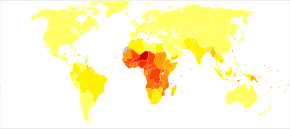
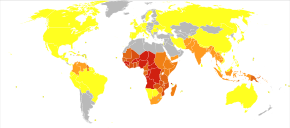
[24][25] In Africa, it is estimated to result in losses of US$12 billion a year due to increased healthcare costs, lost ability to work, and adverse effects on tourism.
[27] The term malaria originates from Medieval Italian: mala aria 'bad air', a part of miasma theory; the disease was formerly called ague or marsh fever due to its association with swamps and marshland.
[15] The presentation may include headache, fever, shivering, joint pain, vomiting, hemolytic anemia, jaundice, hemoglobin in the urine, retinal damage, and convulsions.
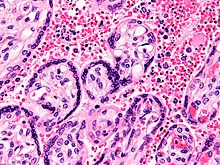
[36] Individuals with cerebral malaria frequently exhibit neurological symptoms, including abnormal posturing, nystagmus, conjugate gaze palsy (failure of the eyes to turn together in the same direction), opisthotonus, seizures, or coma.
For example, in China—whose government in 2010 announced a strategy to pursue malaria elimination in the Chinese provinces—the required investment is a small proportion of public expenditure on health.
Giving children with anaemia in these areas preventive antimalarial medication improves red blood cell levels slightly but does not affect the risk of death or need for hospitalisation.
[65][138] An individual can be protected from a P. falciparum infection if they receive about a thousand bites from mosquitoes that carry a version of the parasite rendered non-infective by a dose of X-ray irradiation.
[needs update][144] In 2021, researchers from the University of Oxford reported findings from a Phase IIb trial of a candidate malaria vaccine, R21/Matrix-M, which demonstrated efficacy of 77% over 12-months of follow-up.
Unlike GSK's RTS,S (AS01) and Serum Institute of India's R21/MatrixM, BNT-165 is being studied in adult age groups meaning it could be developed for Western travelers as well as those living in endemic countries.
[162][163][164] Artemisinin-naphthoquine combination therapy showed promising results in treating falciparum malaria but more research is needed to establish its efficacy as a reliable treatment.
[47] To manage the cerebral malaria when confirmed the following can be done: There is insufficient evidence to show that blood transfusion is useful in either reducing deaths for children with severe anaemia or in improving their haematocrit in one month.
For example, several cities in the Greater Mekong Subregion of Southeast Asia are essentially malaria-free, but the disease is prevalent in many rural regions, including along international borders and forest fringes.
[236] However, factors that contribute to how rainfall results in water for mosquito breeding are complex, incorporating the extent to which it is absorbed into soil and vegetation for example, or rates of runoff and evaporation.
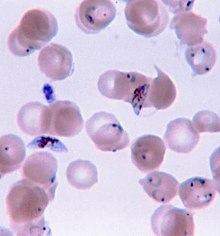
[247][248] Scientific studies on malaria made their first significant advance in 1880, when Charles Louis Alphonse Laveran—a French army doctor working in the military hospital of Constantine in Algeria—observed parasites inside the red blood cells of infected people for the first time.
A year later, Carlos Finlay, a Cuban doctor treating people with yellow fever in Havana, provided strong evidence that mosquitoes were transmitting disease to and from humans.
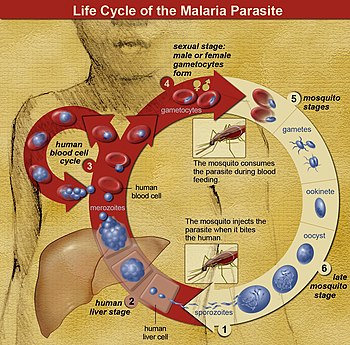
This visit was the start of four years of collaboration and fervent research that culminated in 1897 when Ross, who was working in the Presidency General Hospital in Calcutta, proved the complete life-cycle of the malaria parasite in mosquitoes.
After resigning from the Indian Medical Service, Ross worked at the newly established Liverpool School of Tropical Medicine and directed malaria-control efforts in Egypt, Panama, Greece and Mauritius.
[264][265] Artemisinins, discovered by Chinese scientist Tu Youyou and colleagues in the 1970s from the plant Artemisia annua, became the recommended treatment for P. falciparum malaria, administered in severe cases in combination with other antimalarials.
[103] Before DDT, malaria was successfully eliminated or controlled in tropical areas like Brazil and Egypt by removing or poisoning the breeding grounds of the mosquitoes or the aquatic habitats of the larval stages, for example by applying the highly toxic arsenic compound Paris Green to places with standing water.
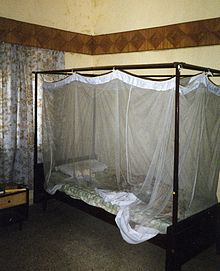
These include antimalarial drugs to prevent or treat infection; improvements in public health infrastructure to diagnose, sequester and treat infected individuals; bednets and other methods intended to keep mosquitoes from biting humans; and vector control strategies[277] such as larvaciding with insecticides, ecological controls such as draining mosquito breeding grounds or introducing fish to eat larvae and indoor residual spraying (IRS) with insecticides.
[282] Experts tie malarial resurgence to multiple factors, including poor leadership, management and funding of malaria control programs; poverty; civil unrest; and increased irrigation.
[281][287] Due to vector and parasite resistance and other factors, the feasibility of eradicating malaria with the strategy used at the time and resources available led to waning support for the program.
[299] Additionally, UNICEF reported that the number of malaria deaths for all ages increased by 10% between 2019 and 2020, in part due to service disruptions related to the COVID-19 pandemic, before experiencing a minor decline in 2021.
[300] Six countries, the United Arab Emirates, Morocco, Armenia, Turkmenistan, Kyrgyzstan, and Sri Lanka managed to have no endemic cases of malaria for three consecutive years and certified malaria-free by the WHO despite the stagnation of the funding in 2010.
World class experts (41 of them) in fields such as malariology, biomedicine, economics and health policy advocated more funding, a central data repository for dealing with local outbreaks of malaria, and training the workers needed to carry out the plan.
[340] In research conducted in 2019, using experimental analysis with knockout (KO) mutants of Plasmodium berghei, the authors were able to identify genes that are potentially essential in the liver stage.
[346] In one study, a genetically modified strain of Anopheles stephensi was created that no longer supported malaria transmission, and this resistance was passed down to mosquito offspring.
[347] Gene drive is a technique for changing wild populations, for instance to combat or eliminate insects so they cannot transmit diseases (in particular mosquitoes in the cases of malaria,[348] zika,[349] dengue and yellow fever).
Its known that plant sugars are the primary source of nutrients for survival of adult mosquitoes,[357] therefore utilising this link for management of the vector will contribute in mitigating malaria transmission.