Rhinoplasty
Rhinoplasty may remove a bump, narrow nostril width, change the angle between the nose and the mouth, or address injuries, birth defects, or other problems that affect breathing, such as a deviated nasal septum or a sinus condition.
The illustrations featured a re-attachment rhinoplasty using a biceps muscle pedicle flap; the graft attached at 3-weeks post-procedure; which, at 2-weeks post-attachment, the surgeon then shaped into a nose.
[10][11] In Germany, rhinoplastic technique was refined by surgeons such as the Berlin University professor of surgery Karl Ferdinand von Gräfe (1787–1840), who published Rhinoplastik (Rebuilding the Nose, 1818) wherein he described 55 historical plastic surgery procedures, and his technically innovative free-graft nasal reconstruction (with a tissue-flap harvested from the patient's arm), and surgical approaches to eyelid, cleft lip, and cleft palate corrections.
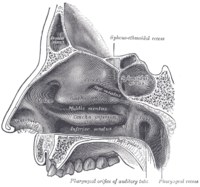
[13][14] In the early 20th century, Freer, in 1902, and Killian, in 1904, pioneered the submucous resection septoplasty (SMR) procedure for correcting a deviated septum; they raised mucoperichondrial tissue flaps, and resected the cartilaginous and bony septum (including the vomer bone and the perpendicular plate of the ethmoid bone), maintaining septal support with a 1.0-cm margin at the dorsum and a 1.0-cm margin at the caudad, for which innovations the technique became the foundational, standard septoplastic procedure.
[15] In 1947, Maurice H. Cottle (1898–1981) endonasally resolved a septal deviation with a minimalist hemitransfixion incision, which conserved the septum; thus, he advocated for the practical primacy of the closed rhinoplasty approach.
The unitary division of the nasal topography permits minimal, but precise, cutting, and maximal corrective-tissue coverage, to produce a functional nose of proportionate size, contour, and appearance for the patient.
The nasal veins are biologically significant, because they have no vessel-valves, and because of their direct, circulatory communication to the cavernous sinus, which makes possible the potential intracranial spreading of a bacterial infection of the nose.
The vomer bone lies below and to the back (posteroinferiorly), and partially forms the choanal opening into the nasopharynx, (the upper portion of the pharynx that is continuous with the nasal passages).
Generally, this area requires an angle greater than 15 degrees for unobstructed breathing; for the correction of such narrowness, the width of the nasal valve can be increased with spreader grafts and flaring sutures.
When observed from below (worm's-eye view), the alar base configures an isosceles triangle, with its apex at the infra-tip lobule, immediately beneath the tip of the nose.
[26][27][28] 3-dimensional cameras allow photographic capture, inspection, analysis, and modification to understand the existing nasal anatomy, and communicate a potential result to the patient.
[33] The plastic surgical correction of congenital and acquired abnormalities of the nose restores functional and aesthetic properties by the surgeon's manipulations of the nasal skin, the subcutaneous (underlying) cartilage-and-bone support framework, and the mucous membrane lining.
[39] The use of piezoelectric instruments requires a more extended approach than the isial one, allowing to visualize the whole bony vault, to reshape it with rhinosculpture or to mobilize and stabilize bones after controlled osteotomies.
In reconstructive rhinoplasty, the defects and deformities that the plastic surgeon encounters, and must restore to normal function, form, and appearance include broken and displaced nasal bones; disrupted and displaced nasal cartilages; a collapsed bridge of the nose; congenital defect, trauma (blunt, penetrating, blast), autoimmune disorder, cancer, intranasal drug-abuse damages, and failed primary rhinoplasty outcomes.
For augmenting the nasal dorsum, autologous cartilage and bone grafts are preferred to (artificial) nose prostheses, because of the reduced incidence of histologic rejection and medical complications.
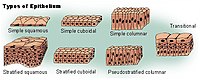
[45] The human nose is a sensory organ that is structurally composed of three types of tissue: (i) an osseo-cartilaginous support framework (nasal skeleton), (ii) a mucous membrane lining, and (iii) an external skin.
The anatomic topography of the human nose is a graceful blend of convexities, curves, and depressions, the contours of which show the underlying shape of the nasal skeleton.
Hence, these anatomic characteristics permit dividing the nose into nasal subunits: (i) the midline (ii) the nose-tip, (iii) the dorsum, (iv) the soft triangles, (v) the alar lobules, and (vi) the lateral walls.
Hence, the rhinoplastic reconstruction of a new nasal subunit, of virtually normal appearance, can be done in a few procedural stages, using intranasal tissues to correct defects of the mucosa; cartilage battens to brace against tissue contraction and depression (topographic collapse); axial skin flaps designed from three-dimensional (3-D) templates derived from the topographic subunits of the nose; and the refinement of the resultant correction with the subcutaneous sculpting of bone, cartilage, and flesh.
Nonetheless, in the final stage of nasal reconstruction—replicating the "normal nose" anatomy by subcutaneous sculpting, the surgeon does have technical allowance to revise the scars, and render them (more) inconspicuous.
Although effective, the bilobed flap technique did create troublesome "dog ears" of excess flesh that required trimming and it also produced a broad skin-donor area that was difficult to confine to the nose.
Said orientations and emplacements eliminated the excess-flesh "dog ears", and thus required a smaller area of donor skin; resultantly, the broad-based, bilobed flap is less prone to the "trap door" and the "pin cushion" deformities common to skin-flap transposition procedure.
[48] The surgeon designs the paramedian forehead flap from a custom-fabricated three-dimensional metal foil template derived from the measures of the nasal defect to be corrected.
The second disadvantage to healing by secondary intention is that the contracture of the wound might distort the normal nasal anatomy, which can lead to a pronounced deformity of the alar rim area.
For this reason, healing by secondary intention generally is not recommended for defects of the distal third of the nose; nonetheless, the exception is a small wound directly upon the nasal tip.
The technical advantages of nasal-defect correction with a skin graft are a brief surgery time, a simple rhinoplastic technique, and a low incidence of tissue morbidity.
Based upon the dimensions (length, width, depth) and topographic locale of the wound and the number of missing nasal-tissue layers, the surgeon determines the rhinoplastic technique for correcting a full-thickness defect; each of the aesthetic nasal subunits is considered separately and in combination.
Furthermore, the medial canthal region is aesthetically hidden by the shadows of the nasal dorsum and of the supraorbital rim, thereby obscuring any differences in the quality of the color and of the texture of the replacement skin (epithelium).
The rhinoplasty patient returns home after surgery, to rest, and allow the nasal cartilage and bone tissues to heal the effects of having been forcefully cut.
Adhesions, scars that obstruct the airways, can form a bridge across the nasal cavity, from the septum to the turbinates, and lead to difficulty breathing and may require surgical removal.











In relation to the nasal bone (teal green), seven bones compose the orbit:
(1) the frontal bone (yellow)
(2) the lacrimal bone (green)
(3) the ethmoid bone (brown)
(4) the zygomatic bone (blue)
(5) the upper jaw maxillary bone (purple)
(6) the palatine bone (aqua)
(7) the sphenoid bone (red)












Nose-narrowing rhinoplasty; two chisel cuts (green and black arrows) meet at the red zig-zag line to release the bone for corrective re-alignment.

The nasal bones (violet) of the dorsum identified, for effecting a nose-narrowing rhinoplasty.
