Pituitary apoplexy
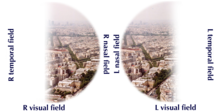
The most common initial symptom is a sudden headache, often associated with a rapidly worsening visual field defect or double vision caused by compression of nerves surrounding the gland.
[1][2][3] Occasionally, the presence of blood leads to irritation of the lining of the brain, which may cause neck rigidity and intolerance to bright light, as well as a decreased level of consciousness.
The fourth (trochlear) and sixth (abducens) cranial nerves are located in the same compartment and can cause diagonal or horizontal double vision, respectively.
This may be caused by low cortisol levels or by inappropriate release of antidiuretic hormone (ADH) from the posterior pituitary.
[2] A quarter has a history of high blood pressure,[1] but this is a common problem in the general population, and it is not clear whether it significantly increase the risk of apoplexy.
[8] Amongst reported associations are surgery (especially coronary artery bypass graft, where there are significant fluctuations in the blood pressure), disturbances in blood coagulation or medication that inhibits coagulation, radiation therapy to the pituitary, traumatic brain injury, pregnancy (during which the pituitary enlarges) and treatment with estrogens.
[3][9] The pituitary gland is located in a recess in the skull base known as the sella turcica ("Turkish saddle", after its shape).
There are various proposed mechanisms by which a tumor can increase the risk of either infarction (insufficient blood supply leading to tissue dysfunction) or hemorrhage.
[4] Larger tumors are more prone to bleeding, and more rapidly growing lesions (as evidenced by detection of increased levels of the protein PCNA) may also be at a higher risk of apoplexy.
[2] After an apoplexy, the pressure inside the sella turcica rises, and surrounding structures such as the optic nerve and the contents of the cavernous sinus are compressed.
[2] If MRI is not suitable (e.g. due to claustrophobia or the presence of metal-containing implants), a computed tomography (CT) scan may demonstrate abnormalities in the pituitary gland, although it is less reliable.
[1] Many pituitary tumors (25%) are found to have areas of hemorrhagic infarction on MRI scans, but apoplexy is not said to exist unless it is accompanied by symptoms.
[1][4] In some instances, lumbar puncture may be required if there is a suspicion that the symptoms might be caused by other problems (meningitis or subarachnoid hemorrhage).
This is the examination of the cerebrospinal fluid that envelops the brain and the spinal cord; the sample is obtained with a needle that is passed under local anesthetic into the spine.
[1] Visual field testing is recommended as soon as possible after diagnosis,[1][4] as it quantifies the severity of any optic nerve involvement, and may be required to decide on surgical treatment.
[4][6] The drug dexamethasone has similar properties,[6] but its use is not recommended unless it is required to reduce swelling in the brain around the area of hemorrhage.
In this procedure, surgical instruments are passed through the nose towards the sphenoid bone, which is opened to give access to the cavity that contains the pituitary gland.
[8] After an episode of pituitary apoplexy, 80% of people develop hypopituitarism and require some form of hormone replacement therapy.
[1][2] The most common problem is growth hormone deficiency, which is often left untreated[1][4] but may cause decreased muscle mass and strength, obesity and fatigue.
Finally, 10–25% develop diabetes insipidus, the inability to retain fluid in the kidneys due to a lack of the pituitary antidiuretic hormone.
[2] Based on extrapolations from existing data, one would expect 18 cases of pituitary apoplexy per one million people every year; the actual figure is probably lower.
[4] The name of the condition was coined in 1950 in a case series by physicians from Boston City Hospital and Harvard Medical School.