Fatty liver disease
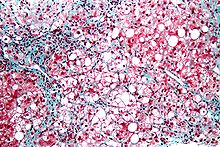
At the beginning, the hepatocytes present small fat vacuoles (liposomes) around the nucleus (microvesicular fatty change).
In this stage, liver cells are filled with multiple fat droplets that do not displace the centrally located nucleus.
In the late stages, the size of the vacuoles increases, pushing the nucleus to the periphery of the cell, giving a characteristic signet ring appearance (macrovesicular fatty change).
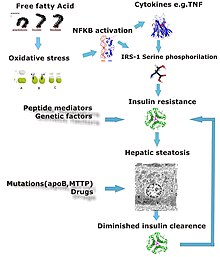
[13][20][21] Defects in fatty acid metabolism are responsible for pathogenesis of FLD, which may be due to imbalance in energy consumption and its combustion, resulting in lipid storage, or can be a consequence of peripheral resistance to insulin, whereby the transport of fatty acids from adipose tissue to the liver is increased.
[13][22] Impairment or inhibition of receptor molecules (PPAR-α, PPAR-γ and SREBP1) that control the enzymes responsible for the oxidation and synthesis of fatty acids appears to contribute to fat accumulation.
Steatosis (retention of lipid) and onset of steatohepatitis may represent successive stages in FLD progression.
[25] The progression to cirrhosis may be influenced by the amount of fat and degree of steatohepatitis and by a variety of other sensitizing factors.
Most individuals are asymptomatic and are usually discovered incidentally because of abnormal liver function tests or hepatomegaly noted in unrelated medical conditions.
Simple blood tests may help to determine the magnitude of the disease by assessing the degree of liver fibrosis.
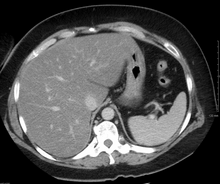
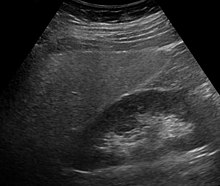
[32] Online calculators have been developed to assist in evaluating hepatic steatosis using CT and MRI findings.
[8] For people with NAFLD or NASH, weight loss via a combination of diet and exercise was shown to improve or resolve the disease.
[8] In more serious cases, medications that decrease insulin resistance, hyperlipidemia, and those that induce weight loss such as bariatric surgery as well as vitamin E have been shown to improve or resolve liver function.
[8][35] In the case of long-term total-parenteral-nutrition-induced fatty liver disease, choline has been shown to alleviate symptoms.
[1] Recently the term Metabolic dysfunction-associated fatty liver disease (MAFLD) has been proposed to replace NAFLD.
MAFLD is a more inclusionary diagnostic name as it is based on the detection of fatty liver by histology (biopsy), medical imaging or blood biomarkers but should be accompanied by either overweight/obesity, type 2 diabetes mellitus, or metabolic dysregulation.
Weight gain was associated with poor adherence to the suggested diet, reduced levels of physical activity, and increased prevalence of homozygosity for the PNPLA3 rs738409 single nucleotide polymorphism.
[45][46] A systematic review and meta-analysis, published in 2024, found that growth hormone therapy may help in the management of fatty liver disease.
[47] Fatty liver disease can occur in pets such as reptiles (particularly turtles[48]) and birds[49] as well as mammals like cats and dogs.