History of medicine
Medical historians often draw from other humanities fields of study including economics, health sciences, sociology, and politics to better understand the institutions, practices, people, professions, and social systems that have shaped medicine.
[20][21] Ancient history covers time between c. 3000 BCE to c. 500 CE, starting from evidenced development of writing systems to the end of the classical era and beginning of the post-classical period.
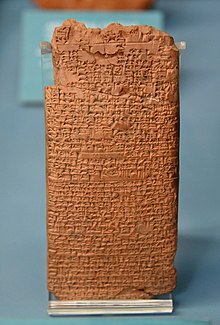
Overlapping ideas of what we now understand as medicine, science, magic, and religion characterised early Mesopotamian healing practices as a hybrid naturalistic and supernatural belief system.
[38] Throughout the civilisations of Mesopotamia there are a wide range of medical innovations, including evidenced practices of prophylaxis, measures to prevent the spread of disease,[28] accounts of stroke,[citation needed] and an awareness of mental illnesses.
It is a text filled with magical charms, spells, and incantations used for various purposes, such as protection against demons, rekindling love, ensuring childbirth, and achieving success in battle, trade, and even gambling.
It also includes numerous charms aimed at curing diseases and several remedies from medicinal herbs, overall making it a key source of medical knowledge during the Vedic period.
The earliest foundations of Ayurveda were built on a synthesis of traditional herbal practices together with a massive addition of theoretical conceptualizations, new nosologies and new therapies dating from about 600 BCE onwards, and coming out of the communities of thinkers which included the Buddha and others.
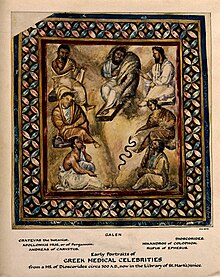
[67][69][70][71] The theory of humors was derived from ancient medical works, dominated Western medicine until the 19th century, and is credited to Greek philosopher and surgeon Galen of Pergamon (129 – c. 216 CE).
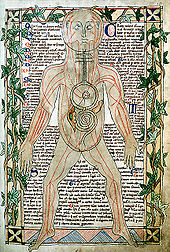
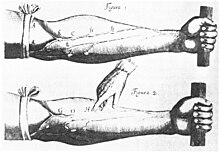
Some of the surgical cures listed, such as the opening of an abdominal abscess or the removal of traumatic foreign material, are realistic enough to have taken place, but with the patient in a state of enkoimesis induced with the help of soporific substances such as opium.
Thus, while working at the medical school of Alexandria, Herophilus placed intelligence in the brain based on his surgical exploration of the body, and he connected the nervous system to motion and sensation.
"[108] The Islamic civilization rose to primacy in medical science as its physicians contributed significantly to the field of medicine, including anatomy, ophthalmology, pharmacology, pharmacy, physiology, and surgery.
Although Islamicate scientists were responsible for discovering much of the knowledge that allows the hospital system to function safely today, European scholars who built on this work still receive the majority of the credit historically.
The Tasrif, written by surgeon Abu Al-Qasim Al-Zahrawi, was translated into Latin; it became one of the most important medical texts in European universities during the Middle Ages and contained useful information on surgical techniques and spread of bacterial infection.
His books (in Latin) covered surgical techniques for many conditions, including hydrocephalus, nasal polyp, goitre and tumours to phimosis, ascites, haemorrhoids, anal abscess and fistulae.
The Florentine Codex, a 16th-century ethnographic research study in Mesoamerica by the Spanish Franciscan friar Bernardino de Sahagún, is a major contribution to the history of Nahua medicine.
In 1847 in Vienna, Ignaz Semmelweis (1818–1865), dramatically reduced the death rate of new mothers (due to childbed fever) by requiring physicians to clean their hands before attending childbirth, yet his principles were marginalized and attacked by professional peers.
In 1860, Pasteur's report on bacterial fermentation of butyric acid motivated fellow Frenchman Casimir Davaine to identify a similar species (which he called bacteridia) as the pathogen of the deadly disease anthrax.
[177] Pettenkofer conceded bacteria's casual involvement, but maintained that other, environmental factors were required to turn it pathogenic, and opposed water treatment as a misdirected effort amid more important ways to improve public health.
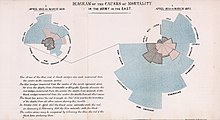
English nurse Florence Nightingale pioneered analysis of large amounts of statistical data, using graphs and tables, regarding the condition of thousands of patients in the Crimean War to evaluate the efficacy of hospital services.
[181][182][183] By the late 19th and early 20th century English statisticians led by Francis Galton, Karl Pearson and Ronald Fisher developed the mathematical tools such as correlations and hypothesis tests that made possible much more sophisticated analysis of statistical data.
[187] This situation was transformed radically from the late eighteenth century as, amid changing cultural conceptions of madness, a new-found optimism in the curability of insanity within the asylum setting emerged.
[190] This new therapeutic sensibility, referred to as moral treatment, was epitomised in French physician Philippe Pinel's quasi-mythological unchaining of the lunatics of the Bicêtre Hospital in Paris[191] and realised in an institutional setting with the foundation in 1796 of the Quaker-run York Retreat in England.
[47] From the early nineteenth century, as lay-led lunacy reform movements gained influence,[192] ever more state governments in the West extended their authority and responsibility over the mentally ill.[193] Small-scale asylums, conceived as instruments to reshape both the mind and behaviour of the disturbed,[194] proliferated across these regions.
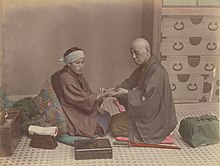
They broke from Japanese traditions of closed medical fraternities and adopted the European approach of an open community of collaboration based on expertise in the latest scientific methods.
The textbook Lehre von den Augenkrankheiten of ophthalmologist Georg Joseph Beer (1763–1821) combined practical research and philosophical speculations, and became the standard reference work for decades.
In Liberia, for example, the United States had large military operations during the war and the U.S. Public Health Service began the use of DDT for indoor residual spraying (IRS) and as a larvicide, with the goal of controlling malaria in Monrovia, the Liberian capital.
By the end of the 20th century, microtechnology had been used to create tiny robotic devices to assist microsurgery using micro-video and fiber-optic cameras to view internal tissues during surgery with minimally invasive practices.
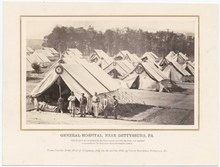
During the 19th century, large-scale wars were attended with medics and mobile hospital units which developed advanced techniques for healing massive injuries and controlling infections rampant in battlefield conditions.
The discovery of penicillin in the 20th century by Alexander Fleming provided a vital line of defence against bacterical infections that, without them, often cause patients to suffer prelonged recovery periods and highly increased chances of death.
This outbreak gave rise to a number of lessons learnt from viral infection control, including more effective isolation room protocols to better hand washing techniques for medical staff.