Vascular surgery
The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs.
[1] Early leaders of the field included Russian surgeon Nikolai Korotkov, noted for developing early surgical techniques, American interventional radiologist Charles Theodore Dotter who is credited with inventing minimally invasive angioplasty (1964), and Australian Robert Paton, who helped the field achieve recognition as a specialty.
Edwin Wylie of San Francisco was one of the early American pioneers who developed and fostered advanced training in vascular surgery and pushed for its recognition as a specialty in the United States in the 1970s.
The most notable historic figure in vascular surgery is the 1912 Nobel Prize winning surgeon, Alexis Carrel for his techniques used to suture vessels.
The field was originally pioneered by interventional radiologists like Dr. Charles Dotter, who invented angioplasty using serial dilatation of vessels.
The surgeon Dr. Thomas J. Fogarty invented a balloon catheter, designed to remove clots from occluded vessels, which was used as the eventual model to do endovascular angioplasty.
The treatment of the aorta, the body's largest artery, dates back to Greek surgeon Antyllus, who first performed surgeries for various aneurysms in the second century AD.
Modern treatment of aortic diseases stems from development and advancements from Michael DeBakey and Denton Cooley.
Dr. Ted Diethrich, one of Dr. DeBakey's associates, went on to pioneer many of the minimally invasive techniques that later became hallmarks of endovascular surgery.
Dietrich trained several future leaders in the field of endovascular surgery at the Arizona Heart Hospital including Venkatesh Ramaiah, MD[3] who succeeded him as medical director of the institution in 2010.
These procedures provide reasonable outcomes that are comparable to surgery with the advantage of short hospital stay (day or overnight for most cases) with lower morbidity and mortality rates.
A recent trend in the United States is the stand-alone day angiography facility associated with a private vascular surgery clinic, thus allowing treatment of most arterial endovascular cases conveniently and possibly with lesser overall community cost.
Disease states generally arise from narrowing of the arterial system known as stenosis or abnormal dilation referred to as an aneurysm.
Other less common causes of stenosis include fibromuscular dysplasia, radiation induced fibrosis or cystic adventitial disease.
Treating aneurysms which involve the ascending aorta are generally within the scope of cardiac surgeons, but upcoming endovascular technology may allow for a more minimally invasive approach in some patients.
The first line treatment for type B aortic dissection is aimed at reducing both heart rate and blood pressure and is referred to as anti-impulse therapy.
Should initial medical management fail or there is the involvement of a major branch of the aorta, vascular surgery may be needed for these type B dissections.
In isolation, visceral artery dissections are discovered incidentally in up to a third of patients and in these cases may be managed medically by a vascular surgeon.
The SMA arises from the abdominal aorta and usually supplies blood from the distal duodenum through two-thirds of the transverse colon and the pancreas.
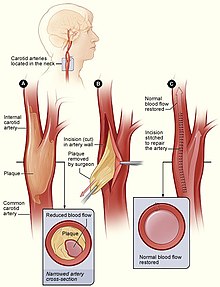
The Society for Vascular Surgery publishes clinical practice guidelines for the management of extracranial cerebrovascular disease.
If there is progression, a patient may also present with chronic limb threatening ischemia which encompasses pain at rest and non-healing wounds.
Vascular surgeons are experts in the diagnosis, medical management, endovascular and open surgical treatment of PAD.
[22] The vascular surgeon has several modalities to treat lower extremity venous disease which including medical, interventional and surgical procedures.
Vascular treatments can include compression stockings, venous ablation or vein stripping, depending on specific patient presentation, severity of disease, among other things.
Minimally invasive diagnostic and therapeutic options might include intravascular ultrasound, venography and iliac vein stenting whereas surgical management may be offered in refractory cases.
[29] Overall, the data shows that there may be a reduction in the incidence in post-thrombotic syndrome in patients who undergo certain procedures for iliofemoral DVT but it is not without risks.
Vascular surgeons may create an AVF for a patient as well as undertake minimally invasive procedures to ensure the fistula remains patent.
For instance, arterial injury in military combatants currently occurs predominantly in males in their twenties who are exposed to improvised explosive devices or gunshot wounds; whereas in the civilian realm, one study conducted in the United States showed the most common mechanisms to include motor vehicle collisions, firearm injuries, stab wounds and falls from heights.
[35] Advances in vascular surgery, specifically endovascular technologies, have led to a dramatic change in the operative approach to blunt thoracic aortic injury (BTAI).
One widely-used classification scheme is based on the extent of injury to the anatomic layers of the aorta as seen with computed tomography angiography or intravascular ultrasound.