Cardiopulmonary bypass
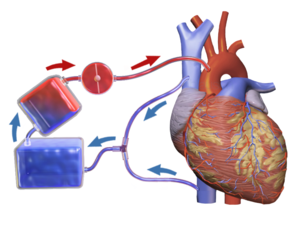
The machine mechanically circulates and oxygenates blood throughout the patient's body while bypassing the heart and lungs allowing the surgeon to work in a bloodless surgical field.
This is to avoid engulfing air systemically, and to provide a bloodless field to increase visibility for the surgeon.
If blood flow is stopped at normal body temperature, permanent brain damage can occur in three to four minutes — death may follow.
The cooled blood slows the body's basal metabolic rate, decreasing its demand for oxygen.
A persistent left superior vena cava may make it difficult to achieve proper venous drainage or deliver of retrograde cardioplegia.
CPB is known to activate the coagulation cascade and stimulate inflammatory mediators, leading to hemolysis and coagulopathies.
For example, when surgeons clamp and connect the aorta to tubing, resulting emboli may block blood flow and cause mini strokes.
[10] The components of the CPB circuit are interconnected by a series of tubes made of silicone rubber or PVC.
By altering the speed of revolution (RPM) of the pump head, blood flow is produced by centrifugal force.
Because hypothermia is frequently used in CPB (to reduce metabolic demands), heat exchangers are implemented to warm and cool blood within the circuit.
[10] Multiple cannulae are sewn into the patient's body in a variety of locations, depending on the type of surgery.
There are multiple types of cardioplegia solutions, but most work by inhibiting fast sodium currents in the heart, which prevent conduction of the action potential.
In particular, the cannulation, cooling, and cardio-protective strategies must be coordinated between the surgeon, anesthesiologist, perfusionist, and nursing staff.
Nonetheless, a surgeon will place a cannula in the right atrium, vena cava, or femoral vein to withdraw blood from the body.
Preoperative imaging or an ultrasound probe may be used to help identify aortic calcifications that could potentially become dislodged and cause an occlusion or stroke.
Once the cannulation site has been deemed safe, two concentric, diamond-shaped pursestring sutures are placed in the distal ascending aorta.
[12] If only a single cannula is to be used (dual-stage cannulation), it is passed through the right atrial appendage, through the tricuspid valve, and into the inferior vena cava.
Setting appropriate blood pressure targets to maintain the health and function of the organs including the brain and kidney are important considerations.
[21] Once the patient is ready to come off of bypass support, the cross-clamp and cannulas are removed and protamine sulfate is administered to reverse the anticoagulative effects of heparin.
The Austrian-German physiologist Maximilian von Frey constructed an early prototype of a heart-lung machine in 1885.
A team of scientists at the University of Birmingham (including Eric Charles, a chemical engineer) were among the pioneers of this technology.
For four years work was undertaken to improve the machine, and on April 5, 1951, Dr. Clarence Dennis led the team at the University of Minnesota Medical Center that conducted the first human operation involving open cardiotomy with temporary mechanical takeover of both heart and lung functions.
The patient did not survive due to an unexpected complex congenital heart defect, but the machine had proved to be workable.
[23][24] One member of the team was Dr Russell M. Nelson, (who later became president of The Church of Jesus Christ of Latter-day Saints), and he performed the first open heart surgery in Utah in November 1951 which was successful.
[25] The first successful mechanical support of left ventricular function was performed on July 3, 1952, by Forest Dewey Dodrill using a machine co-developed with General Motors, the Dodrill-GMR.
[27] Gibbon's machine was further developed into a reliable instrument by a surgical team led by John W. Kirklin at the Mayo Clinic in Rochester, Minnesota in the mid-1950s.
[29] In 1983, Ken Litzie patented a closed emergency heart bypass system which reduced circuit and component complexity.
[30] This device improved patient survival after cardiac arrest because it could be rapidly deployed in non-surgical settings.